TO: Administrative File: CAG-00460N
FROM: Tamara Syrek Jensen, JD
Director, Coverage and Analysis Group
Joseph Chin, MD, MS
Deputy Director, Coverage and Analysis Group
JoAnna Baldwin, MS
Acting Director, Division of Policy and Evidence Review
Andrew Ward, PhD, MPH
Director, Evidence Development Division
David Dolan, MBA
Lead Analyst
Karyn Kai Anderson, PhD, MPH
Epidemiologist
Joseph Dolph Hutter, MD, MA
Lead Medical Officer
SUBJECT: National Coverage Determination for Monoclonal Antibodies Directed Against Amyloid for the Treatment of Alzheimer’s Disease
DATE: April 7, 2022
I. Decision
A. The Centers for Medicare & Medicaid Services (CMS) covers Food and Drug Administration (FDA) approved monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s disease (AD) when furnished in accordance with Section B (Coverage Criteria) under coverage with evidence development (CED) for patients who have:
- A clinical diagnosis of mild cognitive impairment (MCI) due to AD or mild AD dementia, both with confirmed presence of amyloid beta pathology consistent with AD.
B. Coverage Criteria:
1) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) considered as reasonably likely to predict clinical benefit may be covered in a randomized controlled trial conducted under an investigational new drug (IND) application.
2) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit may be covered in CMS approved prospective comparative studies. Study data for CMS approved prospective comparative studies may be collected in a registry.
3) For CMS-approved studies, the protocol, including the analysis plan, must include:
- A study population whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia.
- A neurocognitive evaluation and a description of the instruments used to assess cognition and function for the clinical diagnosis of MCI due to AD or mild AD dementia for study enrollment and outcomes assessment.
- A description of:
- The multidisciplinary dementia team and optimal medical management.
- Study sites with clinical expertise and infrastructure to provide treatments consistent with the safety monitoring outlined in the FDA-approved label.
4) CMS-approved studies of a monoclonal antibody directed against amyloid (antiamyloid mAb) approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit must address all of the questions below:
- Does the antiamyloid mAb meaningfully improve health outcomes (i.e., slow the decline of cognition and function) for patients in broad community practice?
- Do benefits, and harms such as brain hemorrhage and edema, associated with use of the antiamyloid mAb, depend on characteristics of patients, treating clinicians, and settings?
- How do the benefits and harms change over time?
5) CMS-approved studies must adhere to the following standards of scientific integrity that have been identified by the Agency for Healthcare Research and Quality:
- The principal purpose of the study is to test whether the item or service meaningfully improves health outcomes of affected beneficiaries who are represented by the enrolled subjects.
- The rationale for the study is well supported by available scientific and medical evidence.
- The study results are not anticipated to unjustifiably duplicate existing knowledge.
- The study design is methodologically appropriate and the anticipated number of enrolled subjects is sufficient to answer the research question(s) being asked in the National Coverage Determination.
- The study is sponsored by an organization or individual capable of completing it successfully.
- The research study is in compliance with all applicable Federal regulations concerning the protection of human subjects found in the Code of Federal Regulations (CFR) at 45 CFR Part 46. If a study is regulated by the Food and Drug Administration (FDA), it is also in compliance with 21 CFR Parts 50 and 56. In addition, to further enhance the protection of human subjects in studies conducted under CED, the study must provide and obtain meaningful informed consent from patients regarding the risks associated with the study items and/or services, and the use and eventual disposition of the collected data.
- All aspects of the study are conducted according to appropriate standards of scientific integrity.
- The study has a written protocol that clearly demonstrates adherence to the standards listed here as Medicare requirements.
- The study is not designed to exclusively test toxicity or disease pathophysiology in healthy individuals. Such studies may meet this requirement only if the disease or condition being studied is life threatening as defined in 21 CFR §312.81(a) and the patient has no other viable treatment options.
- The clinical research studies and registries are registered on the www.ClinicalTrials.gov website by the principal sponsor/investigator prior to the enrollment of the first study subject. Registries are also registered in the Agency for Healthcare Research and Quality (AHRQ) Registry of Patient Registries (RoPR).
- The research study protocol specifies the method and timing of public release of all prespecified outcomes to be measured including release of outcomes if outcomes are negative or study is terminated early. The results must be made public within 12 months of the study’s primary completion date, which is the date the final subject had final data collection for the primary endpoint, even if the trial does not achieve its primary aim. The results must include number started/completed, summary results for primary and secondary outcome measures, statistical analyses, and adverse events. Final results must be reported in a publicly accessible manner; either in a peer-reviewed scientific journal (in print or on-line), in an on-line publicly accessible registry dedicated to the dissemination of clinical trial information such as ClinicalTrials.gov, or in journals willing to publish in abbreviated format (e.g., for studies with negative or incomplete results).
- The study protocol must explicitly discuss beneficiary subpopulations affected by the item or service under investigation, particularly traditionally underrepresented groups in clinical studies, how the inclusion and exclusion criteria effect enrollment of these populations, and a plan for the retention and reporting of said populations in the trial. If the inclusion and exclusion criteria are expected to have a negative effect on the recruitment or retention of underrepresented populations, the protocol must discuss why these criteria are necessary.
- The study protocol explicitly discusses how the results are or are not expected to be generalizable to affected beneficiary subpopulations. Separate discussions in the protocol may be necessary for populations eligible for Medicare due to age, disability or Medicaid eligibility.
The principal investigator must submit the complete trial protocol, cite where the detailed analysis plan for the CMS CED questions occurs in the protocol, and provide a statement addressing how the study satisfies each of the standards of scientific integrity (a. through m. listed above), as well as the investigator’s contact information, to the email address below. The information will be reviewed, and approved trials will be identified on the CMS website.
Email address for protocol submissions: clinicalstudynotification@cms.hhs.gov Email subject line: "CED Monoclonal Antibodies for the Treatment of Alzheimer’s Disease [name of
sponsor/primary investigator]"
C. Monoclonal antibodies directed against amyloid indicated for the treatment of AD are covered when furnished according to the FDA approved indication in National Institutes of Health (NIH)-supported trials.
D. For any CMS approved study, or NIH-supported trial, that includes a beta amyloid positron emission tomography (PET) scan as part of the protocol, it has been determined that these trials or studies also meet the CED requirements included in the Beta Amyloid Positron Emission Tomography in Dementia and Neurodegenerative Disease NCD (220.6.20).
E. Monoclonal antibodies directed against amyloid for the treatment of AD provided outside of a FDA approved randomized controlled trial, CMS approved studies, or studies supported by the NIH, are nationally non-covered.
Consistent with section 1142 of the Act, AHRQ supports Medicare coverage of FDA trials in Section B.1, NIH trials, and CMS-approved studies that meet all the standards identified above, and address the above-listed research questions.
See Appendix B for the suggested manual language for the National Coverage Determination.
II. Background
Throughout this document we use numerous acronyms, some of which are not defined as they are presented in direct quotations. Please find below a list of these acronyms and corresponding full terminology:
AAN – American Academy of Neurology
AD – Alzheimer’s disease
AFA – Alzheimer’s Foundation of America
AfPA – Alliance for Patient Access
AGS – American Geriatric Society
AHIP – America’s Health Insurance Plan
BIO – Biotechnology Innovation Organization
CDC – Centers for Disease Control and Prevention
CED – Coverage with Evidence Development
CMS – Centers for Medicare & Medicaid Services
CSF – Cerebral spinal fluid
FDA – Food and Drug Administration
GAP – Global Alzheimer’s Platform
IAF – Infusion Access Foundation
IPA – Infusion Providers Alliance
mAbs/mABs – Monoclonal antibodies
MCI – Mild cognitive impairment
MITA – Medical Imaging & Technology Alliance
NAACOS – National Association of ACOs
NAMD – National Association of Medicaid Directors
NCA – National Coverage Analysis
NCD – National Coverage Determination
NDSS – National Down Syndrome Society
NHIA – National Home Infusion Association
NIA – National Institute of Aging
NIH – National Institutes of Health
NMQF – National Minority Quality Forum
PCMA – Pharmaceutical Care Management Association
PhRMA – Pharmaceutical Research and Manufacturers of America
PET – Positron Emission Tomography
SNMMI – Society of Nuclear Medicine and Molecular Imaging
US – United States
A monoclonal antibody directed against amyloid (antiamyloid mAb) for the treatment of AD, is a “biological,” which is a type of drug; the terms “biologicals” and “drugs” are used interchangeably throughout this NCD.
Epidemiology
Alzheimer’s disease (AD) is a currently irreversible brain disorder that progressively degrades memory, cognitive function, and ability to carry out tasks of daily living. AD is the number one cause of dementia in older Americans, contributing to 60-80% of cases. Over 6 million older Americans are believed to have AD. This prevalence is expected to rise to 14 million by 2060 barring effective interventions (such as lifestyle changes, treatment of risk factors, and possibly combinations of Alzheimer’s drugs/biologicals). AD is the sixth leading cause of death in the United States, but may rank from fifth to as high as third (after heart disease and cancer) as a cause of death for older Americans. Older Black individuals are nearly two times as likely to have AD (and other dementias) as older White individuals, and Black patients with AD are more likely to have mixed disease (AD plus one or more other causes of dementia). Older Hispanic individuals are nearly one and one-half times as likely to have AD as older White individuals. Women are more likely to have AD than men, although this is in part because women live longer. (AA 2021, NIA 2021, CDC 2021, Rajan 2021, Brookmeyer 2018, 2019.)
Most individuals with AD become symptomatic after age 65. Alzheimer’s can be fatal anywhere between 2 and 20 years of symptom onset, but 8 years on average (in those with onset before age 75 years). However, pathophysiologic changes in the brain (including amyloid-beta [Aꞵ] plaques and neurofibrillary tangles of tau) may be evident up to decades before symptoms occur. Among 70-year-olds, 61% of those with AD die within a decade (compared to only 30% of those without AD). However, most persons who have evidence of AD pathology but are asymptomatic will not develop AD dementia during their lifetimes. (Ganguli 2005, Brookmeyer 2018, AA 2021, Dilworth 2008, Sperling 2011, CMS 2013, Jack 2010.)
Clinical presentation and progression
The first symptom of AD is usually memory loss (amnesia), due to synaptic dysfunction and loss of neurons in the hippocampus. This leads to impairment of reasoning, judgment, behavior and communication, as well as motor function, as the disease spreads to other regions of brain. Rarely the initial (or "presenting") symptoms can be nonamnestic, such as disturbances in language, visuospatial abilities or decision-making.
Categorizing the onset and progression of AD, and even the definition of AD itself, are subjects of intense debate (Dubois 2021, Jack 2018). Currently there is no universally agreed upon classification system for the "stages" of AD. For example, the Jack 2018 criteria in their Table 6 "bear a close resemblance" to the Global Deterioration Scale (GDS) / Reisberg Scale (seen at https://www.dementiacarecentral.com/aboutdementia/facts/stages/#reisberg). The newer Jack 2018 proposed stages differ in part because they are intended for an amyloid-positive patient population. A recent study by Petersen and colleagues "represents one of the first attempts to fit data into the numeric clinical staging proposed by the [Jack 2018] NIA-AA research framework," and concludes that further modification of these stages is needed (Petersen 2021).
Thus, the categories discussed below: are not meant to resolve ongoing debates about the precise "stages" of AD; recognize that any categorization represents a continuum; and neither assert a particular definition of AD nor are meant to weigh in on the appropriate clinical work up and diagnosis of patients with suspected AD.
Asymptomatic persons with evidence of AD pathology. Termed "preclinical AD" by some, and persons "at-risk for progression to AD" by others, and reflective of "stages 1 and 2" AD, these are persons who are cognitively normal (or at least unimpaired on cognitive tests), but have, at a minimum, pathologic brain amyloid levels as evidenced by PET amyloid, cerebrospinal fluid, or other emerging tests (Jack 2018, Dubois 2021). If these persons have evidence of abnormal tau as well, progression of AD symptomology becomes more likely.
Persons with mild cognitive impairment (MCI) and evidence of AD pathology, termed "prodromal AD" by some, and reflective of "stage 3" AD. MCI is a syndrome in which persons experience memory loss (amnestic MCI) or loss of thinking skills other than memory loss (non-amnestic MCI), to a greater extent than expected for age, but with "minimal impairment of instrumental activities of daily living (IADL)" (Petersen 2018). Risk factors for MCI include advanced age and lower educational status. MCI has multiple subtypes, and while it can be "the first cognitive expression of Alzheimer disease (AD), it can also be secondary to other disease processes (i.e., other neurologic, neurodegenerative, systemic, or psychiatric disorders)" (Petersen 2018). Persons with MCI are at increased risk of developing dementia (whether from AD or another etiology), but many do not progress to dementia, and some get better (those for whom MCI is due to a treatable or self-limiting cause). (Wolk 2009, Hughes 2011, Ward 2012, Landau 2012, Sachdev 2012, Mayo 2021, Petersen 1999, 2009, 2018.)
Persons with dementia and evidence of AD pathology. When persons with MCI and evidence of AD pathology become impaired in performing daily activities, this may indicate onset of AD dementia (reflective of "stage 4" and higher AD). Dementia is a syndrome involving cognitive and behavioral impairment in an otherwise alert patient, due to a number of neurological diseases, alone or combined. Like MCI, dementia is not a specific cause or disease process itself. The dementia impairment must involve a minimum of two domains (memory, reasoning, visuospatial abilities, language or personality behaviors); impact daily functioning; meet other certain criteria; and be objectively documented by a "bedside" mental status exam (e.g., mini-mental status exam, Montreal cognitive assessment) or neuropsychological testing (McKhann 2011, Nasreddine 2005, Mitchell 2009, CMS 2013). We recognize that only patients with mild (as opposed to more severe) dementia are included in contemporary trials; furthermore, trials increasingly focus on individuals who have MCI or are even earlier in the disease process.
Etiology and diagnosis
The underlying cause(s) of AD remain unknown. The number one risk factor is age itself. Other prominent risk factors include genetic predisposition (e.g., the apolipoprotein ε 4 allele, or APOE-ε4), family history of dementia, and risk factors for cardiovascular disease (e.g., high blood pressure, diabetes, obesity, smoking, lack of exercise) (CDC 2021, NIA 2021, AA 2021, CMS 2013.) Investigators hypothesize that a wide range of factors may contribute to the development of AD, including genetic, metabolic, inflammatory and immune system, mitochondrial, environmental, and neuronal, to include both cytoskeletal (occurring within the neuronal cell itself, like tau) and synaptic (altering the connectivity among neurons, like Aβ plaques). (McAlpine 2021, ECRI 2012, Pimplikar 2009, Herrup 2010, Sperling 2011.)
Molecular biomarkers considered hallmarks of AD are Aβ plaques, and neurofibrillary tangles of the protein tau. Neurodegeneration, evidenced by atrophy in specific brain regions on MRI, is a less specific marker, but correlates better with clinical progression of disease; as such, it is the downstream neuronal dysfunction and loss that appear to cause the symptoms of Alzheimer’s disease (Jack 2018, Jack 2011).
Abnormal amyloid is the first known physiological change, giving rise to the amyloid cascade hypothesis, which posits a causal role of amyloid as instigator or essential component of a common pathway (the "central event in the aetiology of Alzheimer's disease") that leads to downstream changes including inflammation, tau pathology, and ultimately neurodegeneration (Alzheimer 1898, 1907; Glenner 1984, Goate 1991, Hardy 1991, Selkoe 1991, Beyreuther 1991, Selkoe and Hardy 2016). The "amyloid hypothesis" itself has evolved into a more contemporary, nuanced form that considers the complexity of newly discovered variables and pathways (Jack 2018, Selkoe and Hardy 2016).
The role of amyloid in Alzheimer’s disease remains complicated for at least three reasons. First, amyloid plaques are seen in other diseases, such as dementia with Lewy bodies, cerebral amyloid angiopathy, Parkinson’s disease, Huntington’s disease, and inclusion body myositis.
Second, amyloid is associated with normal physiologic processes. One author recently summarized: "While Aβ protofibrils and oligomers are known to be toxic (Yakupova 2021, Johannesson 2021), it is now postulated that Aβ is also physiologically produced during neuronal activity (Haass 1992, Kent 2020), augments synaptic plasticity (Finnie 2020) and functions in memory formation (Kent 2020)" (Pleen 2021). Normal function extends to disease prevention or response, such as protection against oxidative stress, regulation of cholesterol transport, and anti-microbial activity. Aβ protects the brain from infections, repairs leaks in the blood–brain barrier, and promotes recovery from injury. In this light, amyloid plaques might even play a protective role early in Alzheimer’s disease. (Esparza 2013, Makin 2018, Guglielmotto 2010, Zou 2002, Yao 2002, Soscia 2010, Puzzo 2015, Shokri-Kojori 2018, Huan 2020.)
Combining the research on amyloid function with the data across multiple anti-amyloid AD trials, one author concludes, ". . . plaque clearance alone does not explain clinical efficacy, and amyloid plaque formation may be a protective mechanism by which soluble oligomers are sequestered to limit their neurotoxicity [Gaspar 2010]" (Tolar 2020). This last point is acknowledged, in part, by contemporary proponents of the amyloid hypothesis; as they state, evidence suggests that "plaques can effectively sequester oligomers in a non-diffusible, less neurotoxic state, at least up to a point" after which "excess oligomers can diffuse onto surrounding synaptic membranes and other hydrophobic cell surfaces (Hong 2014)" (Selkoe and Hardy 2016).
Third, amyloid plaques can be detected in cognitively normal older adults. Autopsy studies demonstrate that approximately one-third of older individuals (20-65% depending on age) who are cognitively normal have amyloid accumulation at levels consistent with AD pathology (Hulette 1998, Price 1999, Knopman 2003, Rowe 2010). Other research however suggests that "[cognitively unimpaired] individuals with abnormal amyloid biomarkers have more rapid progression of atrophy, hypometabolism, and clinical/cognitive decline than individuals without biomarker evidence of Aβ deposition" (Jack 2018).
When a finding of pathologic tau is added to pathologic amyloid (both of which can be detected by PET or in CSF), determination that the disease is consistent with AD becomes more certain. The specificity for diagnosis of AD by detection of both amyloid and tau pathology is still undergoing research (Dubois 2021, Jack 2018). One guideline states unequivocally that "the only disorder that consistently shows an increase in CSF P-tau is AD [Olsson 2016], whereas this biomarker is normal in other neurodegenerative disorders" (Jack 2018). This same guideline further states, "Although it is possible that β-amyloid plaques and neurofibrillary tau deposits are not causal in AD pathogenesis, it is these abnormal protein deposits that define AD as a unique neurodegenerative disease among different disorders that can lead to dementia" (emphasis in the original). This guideline also suggests that research could be effectively guided based on the amyloid + tau + neurodegeneration biomarker data profile of research participants, without presuming to answer definitively the bigger question of causality (Jack 2018).
Even with these advancements in evidence and research guidance since the 2011 NIA-AA guidelines, as a real world, practical matter, clinical diagnosis and possible interventions remain a challenge because most dementias are associated with mixed pathology. The most prevalent co-contributor to cognitive decline (especially early mild decline) appears to be cerebrovascular disease, which includes small vessel ischemia in addition to strokes and microinfarcts. Examples of other co-diseases include: Lewy body disease; frontotemporal lobar degeneration; Parkinson’s disease; and hippocampal sclerosis associated with TAR DNA binding protein 43 (TDP-43) proteinopathy (whether part of, or co-existing with, AD) (Nelson 2019, Brookmeyer 2018, AA 2021, Nag 2015). Autopsy studies support that less than 20 percent of persons with AD have "pure" AD (no mixed pathology), lending credence to the comment that "the least common form of Alzheimer’s disease is Alzheimer’s disease" (Schneider 2007, Wilson 2010, Karlawish 2021a). The impact of these mixed diseases on cognition and functioning may be separate and additive, although "it is uncertain whether multiple mixed pathologies act independently or
synergistically on risk of all cause dementia" (Brookmeyer 2018). The implication is that any treatment targeting amyloid specifically may be less effective the greater the level of mixed disease in a given patient.
In sum: the etiology of AD is unknown and may be multifactorial; clinical diagnosis is poor (Beach 2012, Knopman 2001) and can be improved by biomarkers, but to a degree that is debated; the role of Aꞵ as cause vs marker of disease remains controversial.
Treatment
Currently, there is no effective treatment for AD. Existing medications do not prevent, halt, or slow – let alone reverse – the disease. Care is therefore primarily supportive and increases as functional impairment progresses, eventually leading to round-the-clock supervision which can be needed for years. Some medications, such as memantine and cholinesterase inhibitors, can temporarily improve cognitive and neuropsychiatric symptoms in some patients with AD (as well as certain other dementias) (Birks 2006, Reisberg 2003). Addressing risk factors likely helps. The 2020 Lancet Commission concludes that lifestyle changes and treatment of 12 modifiable risk factors associated with Alzheimer’s could potentially prevent or delay up to 40% of dementia cases (Livingston 2020).
Antiamyloid-beta monoclonal antibodies (antiamyloid mAbs), the treatment considered in this NCD, are laboratory-made proteins designed to bind a specific substance in the body, with the goal of marking it for destruction by the body’s immune system. Scientists design various mAbs as treatments with the goal of targeting and neutralizing or clearing infections (like the COVID-19 virus), cancer cells, and in the case of Alzheimer’s disease, amyloid accumulation in brain.
Aduhelm™ (aducanumab) is the first and only such antiamyloid mAb to be approved by the FDA, and was done so under FDA’s "accelerated approval" pathway. At the time of this NCD analysis, CMS is aware of at least three other antiamyloid mAbs (gantenerumab, donanemab, and lecanemab) currently undergoing Phase 3 trials designed for FDA approval (ClinicalTrials.gov 2022).
III. History of Medicare Coverage
Prior to this NCD analysis, CMS did not have an NCD specific to monoclonal antibodies directed against amyloid for the treatment of AD. In the absence of an NCD, coverage decisions for monoclonal antibodies directed against amyloid for the treatment of AD have been made by local Medicare Administrative Contractors (MACs).
A. Current Request
CMS opened this NCD analysis to complete a thorough review of the evidence to consider coverage of monoclonal antibodies directed against amyloid for the treatment of AD.
B. Benefit Category
Medicare is a defined benefit program. For an item or service to be covered by the Medicare program, it must fall within one of the statutorily defined benefit categories outlined in the Social Security Act.
Monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s Disease may be considered a drug or biological that may fall within the benefit categories under 1861(s)(2)(A) or 1861(s)(2)(B) of the Social Security Act.
IV. Timeline of Recent Activities
V. Food and Drug Administration (FDA) Status
Aduhelm is the only antiamyloid mAb approved by the FDA. On June 7, 2021, the FDA approved aducanumab (brand name Aduhelm) with an indication for use in the treatment of Alzheimer’s disease. On July 7, 2021, the indication for use was updated to clarify that treatment with Aduhelm should be initiated in patients with mild cognitive impairment or mild dementia stage of Alzheimer's disease, the population in which treatment was initiated in clinical trials. The letter is available online: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2021/761178Orig1s003ltr.pdf
VI. General Methodological Principles
When making national coverage determinations, CMS generally evaluates relevant clinical evidence to determine whether or not the evidence is of sufficient quality to support a finding that an item or service falling within a benefit category is reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member. The critical appraisal of the evidence enables us to determine to what degree we are confident that: 1) the specific assessment questions can be answered conclusively; and 2) the intervention will improve health outcomes for beneficiaries. An improved health outcome is one of several considerations in determining whether an item or service is reasonable and necessary.
A detailed account of the methodological principles of study design that the Agency utilizes to assess the relevant literature on a therapeutic or diagnostic item or service for specific conditions can be found in Appendix A.
Public comments sometimes cite published clinical evidence and give CMS useful information. Public comments that give information on unpublished evidence such as the results of individual practitioners or patients are less rigorous and therefore less useful for making a coverage determination. Public comments that contain personal health information that cannot be redacted will not be made available to the public. CMS responds in detail to the public comments on a proposed national coverage determination when issuing the final national coverage determination.
VII. Evidence
A. Introduction
This section provides a summary of the evidence we considered during our review. The evidence reviewed to date includes the published medical literature on pertinent clinical trials of monoclonal antibodies directed against amyloid for the treatment of AD. Our assessment focuses on the key evidence question below.
B. Discussion of Evidence
1. Evidence Question
Is the evidence sufficient to conclude that the use of monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s disease improves health outcomes for Medicare beneficiaries?
2. External Technology Assessments
CMS did not request an external technology assessment (TA) on this issue.
3. Internal Technology Assessment
We searched the data bases Academic Search Premier, CINAHL, Google Scholar, Ovid Medline, PubMed, Scopus, and Web of Science, for English language articles in peer-reviewed journals, published from 2010 – 2021, using the search terms ‘Phase 3 Clinical Trials’, ‘beta-Amyloid’, and ‘monoclonal antibodies. To ensure that we captured all the relevant articles, the search was conducted independently and concurrently by a NIH librarian, the contractor International Consulting Associates (ICA), and CAG. As the searches were completed, the NIH librarian first, ICA second, and CAG last, we incorporated all the distinct, relevant references into a single reference database. The final result was the identification of over 300 peer-reviewed documents relevant to the NCD analysis.
These searches resulted in over 300 articles, including descriptions and assessments of Phase 3 clinical trials testing the efficacy and safety of using monoclonal antibodies for treatment of Alzheimer’s Disease (AD). Some of the studies, such as Konstantinos Avegerinos et al., "Effects of monoclonal antibodies against amyloid-β on clinical and biomarker outcomes and adverse risks: A systematic review and meta-analysis of phase III RCTs in Alzheimer’s disease," a 2021 publication in Aging Research Reviews, were metanalyses that surveyed multiple clinical trials testing a variety of potential anti-amyloid drugs for treatment of AD. In addition to peer-reviewed articles, we reviewed reports from other agencies, including the FDA, the Guideline Development, Dissemination and Implementation Subcommittee of the American Academy of Neurology, the National Institute on Aging, and the National Institute for Health Care and Excellence. We also reviewed the Institute for Clinical and Economic Review’s May 5, 2021 report "Aducanumab for Alzheimer’s Disease: Effectiveness and Value."
4. Medicare Evidence Development & Coverage Advisory Committee (MEDCAC)
A MEDCAC meeting was not convened on this issue.
Below are two Evidence Tables.
Table 1 contains summary descriptive information about individual Phase 3 RCTs.
Table 2 contains summary results from Phase 3 RCTs.
To ensure the public has access to the same information that CMS reviewed, we included the national clinical trial (NCT) numbers that uniquely identify all of the RCTs (12) for both tables. To review the trials, go to clinicaltrials.gov and enter the NCT number into the search box under "Other terms." The tables also include, for each row, the author name and year. The full citation for the publication can be found in the bibliography of this decision memorandum which will allow anyone to find the information reviewed by CMS.
Evidence Table 1. Individual Phase-3 RCTs of monoclonal antibodies versus placebo in Alzheimer’s Disease: Summary-level information
Evidence Table 2. Individual Phase 3 RCTs, and meta-analyses, of monoclonal antibodies versus placebo in Alzheimer’s Disease: Random effects modeling results (standardized mean difference (SMD) and 95% confidence interval, unless otherwise noted) for all outcomes, with only statistically significant results presented, and related author-attributed effect sizes, when availablea
VIII. Public Comment
CMS uses the initial public comments to inform its proposed decision. CMS responds in detail to the public comments on a proposed decision when issuing the final decision memorandum. All comments that were submitted without personal health information may be viewed in their entirety by using the following link https://www.cms.gov/medicare-coverage-database/view/ncacal-public-comments.aspx?ncaid=305&ncacaldoctype=all&status=all&sortBy=status&bc=17.
Initial Comment Period: 07/12/2021 – 08/11/2021
During the 30-day comment period following the release of the tracking sheet, CMS received 131 comments. The majority of comments, approximately 77 commenters, did not support coverage or recommended coverage with evidence development (CED). Twenty-six comments did not state a clear position regarding coverage.
The comments included 58 from physicians, and eight from medical companies. We also received 26 comments on behalf of national associations/professional societies, including the American Academy of Neurology (AAN), UsAgainstAlzheimer’s, Biotechnology Innovation Organization (BIO), Public Citizen, Value Based Care Coalition, National Home Infusion Association (NHIA), Medical Imaging & Technology Alliance (MITA), National Association of ACOs (NAACOS), National Association of Medicaid Directors (NAMD), America’s Health Insurance Plans (AHIP), Society of Nuclear Medicine and Molecular Imaging (SNMMI), Alzheimer’s Association, National Minority Quality Forum (NMQF), Alliance for Patient Access (AfPA), Global Alzheimer’s Platform (GAP), American Geriatrics Society (AGS), Infusion Providers Alliance (IPA), Alliance for Aging Research, National Down Syndrome Society (NDSS), Duke Margolis Center for Health Policy, Alzheimer’s Foundation of America (AFA), Infusion Access Foundation (IAF), Pharmaceutical Care Management Association (PCMA), Pharmaceutical Research and Manufacturers of America (PhRMA).
In addition to the above public comments, CMS held two stakeholder meetings and met with numerous patient advocates organizations, manufactures, payers, and think tanks. See the mAb Tracking Sheet (https://www.cms.gov/medicare-coverage-database/view/ncacal-tracking-sheet.aspx?ncaid=305&ncacaldoctype=all&status=all&sortBy=status&bc=17) for the stakeholder meeting transcripts and a full list of the organizations.
The themes from the comments included criticism of the evidence for Aduhelm™, citing conflicting results between EMERGE and ENGAGE, and the presence of adverse events (e.g., Amyloid Related Imaging Abnormalities (ARIA)). The commenters cited that these are reasons additional evidence is needed before the drug is coverable, or expressing that coverage should be limited to CED. Commenters also expressed concerns over the price of Aduhelm™. Commenters stated that CMS should cover Aduhelm™, and future anti-amyloid monoclonal antibodies, based on FDA approval and because of the lack of available effective treatments for AD. Commenters specified that diagnostic tests for beta amyloid should also be included in coverage.
Second Comment Period: 01/11/2022 – 02/10/2022
During the 30-day public comment period following the release of the proposed NCD and decision memorandum, CMS received over 10,000 comments. Of these comments, 68 were omitted from publication on the CMS website due to excessive personal health information content, for a total of 9,957 comments posted to the CMS website. None of the comments included new evidence that met our inclusion/exclusion criteria. However, Biogen’s recent publication of its EMERGE and ENGAGE trial results was reviewed
as well as the new American Academy of Neurology (AAN)guidelines. All comments were considered for this final decision and are summarized in the comments and responses below.
The majority of comments, approximately 65 %, stated that there was not enough evidence to cover antiamyloid mAbs. These commenters either supported the proposed CED decision for antiamyloid mAbs, or stated that antiamyloid mAbs should not be covered by CMS. Of these comments, over 5,000 were form letters, where at least part of the comment contained nearly identical language regarding the evidence and the request for CMS to exclude Aduhelm from coverage. CMS also received around 700 comments
expressing support for coverage of antiamyloid mAbs, with many stating that CMS has previously covered treatments for conditions such as HIV and cancer that had been approved by the FDA under accelerated approval. Many of these commenters also mentioned the lack of alternative treatment options and that coverage limited to only randomized controlled trials would be duplicative of studies required for the FDA and would further limit patient access. The remaining comments (approximately 2,700) did not express clear support for coverage, non-coverage, or coverage under CED. About 60% of these comments were from stakeholders requesting that patients with Down syndrome and other intellectual and developmental disabilities (IDD) have the same access other patients would have to antiamyloid mAbs, while several other commenters mentioned that Medicare should negotiate drug prices. Some comments were also specific to the PET for beta amyloid requirement in the proposed decision.
While CMS received a record number of comments on the proposed NCD and decision memorandum, many of these comments included very similar details and requests. All of the comments received are reflected in the comment and responses to the themes below:
Lack of Evidence for Clinical Benefit
Comment: The majority of public comments stated that that there is not enough evidence showing that these drugs/biologicals provide a clinical benefit in order to cover antiamyloid mAbs.
Response: CMS appreciates these comments and believe that CED as modified in this final decision is the right balance of providing appropriate patient access and patient protections as well as generating evidence needed for patients, clinicians and caregivers.
Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of Alzheimer’s disease based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) considered as reasonably likely to predict clinical benefit
Comment: Several commenters stated that CMS should not restrict access to an FDA approved treatment for AD, especially since there are no alternative options available.
Response: We appreciate these comments and recognize that Alzheimer’s disease is a significant burden affecting the Medicare population. However, currently no Alzheimer’s drug of any type has succeeded, to date, in modifying disease progression. No trial involving any intervention, alone or combined, has yet demonstrated a meaningful improvement in health outcomes for patients treated with antiamyloid mAbs for the treatment of AD. More trials are needed, and the results of these trials will assist in providing answers to CMS, as well as to clinicians, patients, and caregivers, regarding the clinical benefits and harms of this treatment. Based on public comments, we balanced providing patient access, patient protections and generating evidence to answer the questions that are key to helping patients, caregivers, and clinicians making decisions about the best treatments for each individual.
Coverage with Evidence Development (CED) Randomized Controlled Trial requirement
Comment: Several commenters stated that the requirement of a randomized controlled trial for a drug that has been approved by the FDA is unprecedented, with some questioning CMS’ authority for such a requirement.
Response: CMS, historically, has completed few NCDs for drugs or biologics. The reason for this is not because of a single factor. Most drugs/biologics are based on at least two RCTs or based on an intermediate/surrogate outcome that has shown a clear connection to a clinical benefit (e.g., lowering blood pressure reduces chance of stroke, reducing tumor size and mortality). As stated in the analysis, for these particular class of drugs/biologics, there is currently no Alzheimer’s drug of any type that has succeeded, to date, in modifying disease progression. No trial involving any intervention, alone or combined, has yet demonstrated a meaningful improvement in health outcomes for patients treated with antiamyloid mAbs for the treatment of AD. More trials are needed, and the results of these trials will assist in providing answers to CMS, as well as to clinicians, patients, and caregivers, regarding the clinical benefits and harms of this treatment.
In proposing and finalizing this NCD and decision memorandum, CMS followed a long-standing process established by Congress in making an NCD under section 1862(l) of the Act. We have looked to the medical and scientific evidence and found that this treatment could not be covered under the reasonable and necessary standard in section 1862(a)(1)(A). However, we believe it is appropriate to support further research in this area given that AD is a particularly important condition affecting the aged Medicare population. We worked closely with AHRQ about the appropriate standards for the clinical studies that would be necessary to answer the remaining scientific and medical questions. The results of these studies may result in sufficient evidence to expand Medicare coverage in the future. Coverage in the context of ongoing clinical research protocols or with additional data collection can expedite earlier beneficiary access to innovative technology while ensuring that systematic patient safeguards, including assurance that the technology is provided to clinically appropriate patients, are in place to reduce the risks inherent to new technologies, or to new applications of older technologies.
While this is the first time CMS had proposed to cover a drug/biologic through Coverage with Evidence Development (CED) with a randomized controlled trial requirement, CMS has finalized other National Coverage Determinations (NCDs) for drugs/biologics with CED. For example, under the NCD for Beta Amyloid Positron Tomography in Dementia and Neurodegenerative Disease (NCD 220.6.20), the CED requirement for positron emission tomography beta amyloid imaging (which uses radiopharmaceuticals) can be met by comparative and longitudinal clinical trials. Another example is that the NCD for Stem Cell Transplantation (NCD 110.23) requires prospective clinical studies. Randomized controlled trials are not required under those NCDs, but CMS has required randomized controlled trials in other NCDs, including for FDA-approved uses in some cases. For example, the NCD for Vagus Nerve Stimulation (VNS) for Treatment Resistant Depression (TRD) (NCD 160.18) provides coverage under CED in a CMS approved, double-blind, randomized, placebo-controlled trial.
Comment: Many commenters suggested covering antiamyloid mAbs only in randomized controlled trials is duplicative of trials required by the FDA that are designed to answer the question of clinical benefit. CMS should not require the same RCTs as the FDA.
Response: Informed by public comments, our current approach to CED for antiamyloid mAbs is similar to, but has evolved from, our January 2022 proposed NCD and decision memorandum. Many commenters agree with the FDA (and the CMS proposed decision) that there needs to be clear (nonconflicting) evidence of clinical benefit associated with use of an antiamyloid mAb for patients with early AD. We recognize that confirmatory trials required by the FDA for antiamyloid mAbs are designed to determine whether that drug/biologic provides a clinical benefit. Therefore, CMS has agreed to modify the final decision to specify that monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) may be covered in a randomized controlled trial conducted under an investigational new drug (IND) application.
CMS does not require a separate RCT that duplicates an RCT conducted for FDA approval. We removed the "CMS-approved trial" language to further avoid any confusion with regard to CMS’ intent to support FDA required RCTs. At the time of this writing, Aduhelm would be eligible for Medicare coverage in any FDA approved trial. As part of coverage, routine items and services would also be coverable without any further action by CMS.
Comment: Many commenters did not agree with the requirement that all trials must be conducted in a hospital-based outpatient center, stating that this would further restrict access for patients in underserved areas and discriminates against independent outpatient infusion centers.
Response: The final decision reflects the public comments requesting CMS to expand the place of service beyond hospital-based outpatient centers. CMS is not restricting the place of service in the final NCD.
In the proposed decision, we expressed that approved clinical trials should remain in hospital-based outpatient facilities to ensure integrated and coordinated care, availability of advanced imaging or other diagnostic tests, and rapidly-available advanced care if needed. These continue to be important factors for optimized patient health outcomes. Based on public comment, we do not restrict the place of setting in this final decision to ensure that antiamyloid mAbs that have received FDA approval based upon evidence of efficacy from a direct measure of clinical benefit may be given to a broader patient population which is important to answer the first CED question regarding Medicare patient outcomes in broader community settings. To ensure there continues to be integrated and coordinated advanced care, if needed, CMS is requiring that any clinical study protocol submitted for CMS-approval include a description of the multidisciplinary dementia team and optimal medical management of patients, and the study sites with clinical expertise and infrastructure to provide treatments consistent with the safety monitoring outlined in the FDA-approved label. This protocol requirement will ensure the highest level of appropriate clinical care, and to reassure patients and their caregivers that further research with antiamyloid mAbs will be conducted in a rigorous setting to minimize potential harms from the treatment.
We believe all FDA-approved randomized controlled trials and NIH trial have the all appropriate safeguards for patients.
Comment: Some commenters stated that the CED requirement would hurt future innovation for Alzheimer’s disease treatments.
Response: CMS does not agree with these comments. We believe by defining the criteria by which a forthcoming therapy for Alzheimer’s disease could be covered would actually facilitate innovation. The CMS final decision gives the public a clear definition of where the goal line is for what constitutes success in a trial (and thus what meets the standard for "reasonable and necessary" required by law). Medical innovation must include clinical trials that demonstrate benefit to patients. Conversely,
covering a drug that has not been shown to be effective may incentivize production, marketing and sales of similarly ineffective drugs, at the cost of hard research to find ones that do provide a clinical benefit to patients.
Antiamyloid mAbs as a Class
Comment: Many commenters stated that the proposed CED NCD should be specific to Aduhelm only.
Response: This NCD takes a class approach, similar to other NCDs, in order to create a predictable pathway to national coverage that applies to every drug in this antiamyloid mAb class. As discussed in the Analysis of this decision memorandum, the antiamyloid drugs/biologicals have a similar function of reducing amyloid in the brain in the hopes it will slow down the progression of AD. There are other antiamyloid mAbs currently conducting Phase 3 trials (see clinicaltrials.gov). While the evidence based on published trials (Phase 2 and 3) has failed to establish a meaningful clinical benefit associated with the use of any monoclonal antibody directed against AD, the nature of the evidence regarding health outcomes is the same for all mAbs described in the literature. In particular, what is common to all monoclonal antibodies directed against AD (aducanumab, donanemab, lecanemab, and others) is that, in varying degrees, they have been shown to reduce amyloid levels. Thus, given the similar function, treatment uses and current state of evidence, it is consistent to address these mAbs as a particular class.
At the same time, as each antiamyloid mAb in this class may have a distinct mechanism of action resulting in a distinct benefit/risk profile, each will be evaluated on its own merit in its own studies. This position on individual drug evaluation has been consistently promoted by manufacturers and other experts; we agreed in our proposed decision, and continue to agree in this final decision. Our position is also aligned with the FDA’s: each antiamyloid mAb is evaluated in its own RCTs for the FDA. CMS is committed to quickly reconsidering this NCD once an antiamyloid drug has answered the CED questions with quality evidence.
Comment: Some commenters suggested that a decision for the entire class of drugs/biologics is premature given the antiamyloid mAbs that are currently in development.
Response: CMS is issuing a final NCD on the class of drugs/biologics because even if FDA were to determine that an antiamyloid mAb drug/biologic is approved because it demonstrates efficacy from a direct measure of clinical benefit, the approval is based on RCT results in rigorous settings such as academic centers, with dementia experts and patients that have fewer co-morbidities than the general Medicare population. It is important that there is evidence that demonstrates that the positive RCT results from FDA approval are generalizable to the broader Medicare population that include patients with co-morbidities, such as hypertension, heart disease, diabetes, etc. At this time, CMS believes an FDA determination of a drug/biologic that demonstrates efficacy from a direct measure of clinical benefit is promising but does not meet the 1862(a)(1)(A) reasonable and necessary statute. A prospective comparative study, which could range from a registry with a comparator to a pragmatic clinical study is appropriate coverage until CMS knows that the drug/biologic will demonstrate the same health outcomes, with reasonable risk of harm in broad community practice.
Publishing the CMS coverage criteria creates a predictable pathway to Medicare coverage for any antiamyloid mAb that meets the coverage criteria specified in Section I of this NCD. Under the final NCD, manufacturers or other stakeholders working with CMS will be able to ensure access to antiamyloid mAb expeditiously once a drug/biologic has FDA approval and if it meets the coverage criteria outlined in Section I of this decision memorandum. CMS believes that manufacturers and other stakeholders have enough notice to develop a study that provide access in broad community settings to an antiamyloid mAb expeditiously after FDA approval. CMS has also articulated its expectations regarding the level of evidence that each antiamyloid mAb must meet to obtain coverage under 1862(a)(1)(A) of the Act. Stakeholders have asked for this type of information over the years.
We also note that CED does not mean there will be no access to the drug. Once a drug has demonstrated clinical benefit, a prospective comparative study in a community setting could include large number of Medicare patients.
Comment: Some commenters recommended that the CMS coverage decision should be limited to only antiamyloid mAbs that are approved under the FDA accelerated approval pathway. An additional randomized controlled trial, outside of the FDA required confirmatory trial, should not be a Medicare requirement.
Response: Informed by public comments, our current approach to CED for antiamyloid mAbs is similar to, but has evolved from, our January 2022 proposed NCD and decision memorandum. Many commenters agree with the FDA (and the CMS proposed decision) that there needs to be clear (nonconflicting) evidence of clinical benefit associated with use of an antiamyloid mAb for patients with early AD. However, CMS continues to believe, in order to establish a predictable pathway to national coverage it must apply to every drug in this antiamyloid mAb class and apply throughout the product cycle until there is evidence-supported answers to the CED questions. CMS has also articulated its expectations for coverage that each antiamyloid mAb must meet to obtain coverage under 1862(a)(1)(A) of the Act which stakeholders have advocated for over the years.
This final NCD does not apply only to antiamyloid mAbs that obtained FDA-approval based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) considered as reasonably likely to predict clinical benefit. The final NCD also provides coverage for antiamyloid mAbs that have FDA approval based upon evidence of efficacy from a direct measure of clinical benefit. As stated earlier, under the final NCD framework, CMS has ensured expeditious access to antiamyloid mAb as soon as FDA approval if it meets the coverage criteria outlined in Section I of this decision memorandum. This NCD creates 1) support, without interfering with, FDA and NIH trials of FDA-approved antiamyloid mAbs when that support is sought, 2) when an antiamyloid mAb is approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit, CMS supports Medicare beneficiaries who are similar to those trial patients to have access to that drug/biologic in prospective comparative studies and 3) along with this expeditious, appropriate access, CMS wants simultaneous obtain data from quality studies that answer the CED questions (see Section I for the CED questions). This data will be essential for Medicare beneficiaries and their referring and treating physicians to make informed, appropriate decisions about use of the drug.
Comment: Public commenters stated that if an antiamyloid mAb demonstrates a meaningful clinical benefit, that future antiamyloid mAbs should be covered.
Response: We agree that if an antiamyloid mAb demonstrates a clinical meaningful benefit it should be covered by Medicare. At this time there is no antiamyloid that does demonstrate a clinically meaningful benefit. Further, even if FDA were to determine that an antiamyloid mAb drug/biologic is approved because it demonstrates efficacy from a direct measure of clinical benefit, the approval is based on RCT results in rigorous settings such as academic centers, with dementia experts and patients that have fewer co-morbidities than the general Medicare population. It is important that there is evidence that demonstrates that the RCT results from FDA approval are generalizable to the broader Medicare population that include patients with co-morbidities, such as hypertension, heart disease, diabetes, etc. At this time, CMS believes an FDA determination of a drug/biologic that demonstrates efficacy from a direct measure of clinical benefit would be promising but would not meet the 1862(a)(1)(A) reasonable and necessary statute. A prospective comparative study, which could range from a registry with a comparator to a pragmatic clinical study is appropriate coverage until CMS knows that the drug/biologic will demonstrate the same health outcomes, with reasonable risk of harm in broad community practice.
With the goal of providing appropriate coverage for Medicare beneficiaries seeking treatment for MCI and mild AD, CED is the right first step because it balances beneficiary access, beneficiary protections and evidence development to answer the CED questions in Section I, Final Decision and further explained in Section IX, Analysis of this decision.
By creating an NCD for all antiamyloid mAbs in a particular class for treating AD we are establishing a predictable pathway to national coverage for Medicare beneficiaries. CMS has also articulated its expectations for coverage that each antiamyloid mAb must meet to obtain coverage under 1862(a)(1)(A) of the Act. Stakeholders have asked for this type of information over the years.
We note, as we stated above, that CED does not equate to no or little access once the antiamyloid mAb is approved by the FDA for the treatment of AD based on the evidence of efficacy from a direct measure of clinical benefit. Once a drug/biologic has demonstrated clinical benefit as determined under the FDA standard, a prospective study in a community setting could include larger numbers of Medicare patients.
Comment: Some commenters suggested alternative study designs that are less rigorous, such as observational studies.
Response: For antiamyloid mAbs drugs/biologics that have been approved by the FDA for the treatment of AD based upon evidence of efficacy from a change in surrogate endpoint (e.g., amyloid reduction) considered reasonably likely to predict clinical benefit, the NCD will provide coverage in a randomized controlled trial conducted under an investigational new drug application.
Antiamyloid mAbs approved by FDA for the treatment of AD based on the evidence of efficacy from a direct measure of clinical benefit may be covered in CMS approved prospective comparative studies to answer the CED questions specified in Section 1 of this NCD. Prospective comparative studies encompass a variety of study designs including pragmatic randomized trials, and all study data may be collected in a registry. The degree of rigor in the CED study design for a particular antiamyloid mAb will be determined in large part by the strength of evidence in the initial, successful trial(s) designed for FDA approval of that particular drug. It will be the manufacturer or other stakeholders' responsibility to develop a protocol that meets the requirements in this decision and be rigorous enough to answer the CED questions. We believe the studies CMS will approve can allow broader access, while protecting beneficiaries and generating important evidence.
Health Equity
Comment: Many commenters were supportive of the requirement in the proposed decision which specified that the diversity of patients included in each trial must be representative of the national population diagnosed with AD.
Response: CMS appreciates these comments. CMS remains committed to the advancement of health equity by addressing the health disparities that underlie our health system. The requirements of the final NCD directly address this underrepresentation by proposing an unprecedented level of diversity in these clinical trials. We updated the current language regarding diversity of patients to state that the study must include a population whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia.
Comment: Commenters mentioned that while the proposed decision specifies a diversity requirement, only covering antiamyloid mAbs in randomized controlled trials would actually worsen health equity issues due to the relatively small number of patients that would be enrolled in these trials, and the location of study sites away from rural areas.
Response: We continue to believe that the FDA RCTs conducted under an IND application are most appropriate when an antiamyloid mAb is FDA approved based upon evidence of efficacy from a change in surrogate endpoint (e.g., amyloid reduction). If an antiamyloid mAb is approved by FDA for the treatment of AD based on the evidence of efficacy from a direct measure of clinical benefit, we are expanding the NCD to include CMS approved prospective comparative studies. The expanded coverage (compared to the proposed determination) will provide an opportunity for broader access. These studies are not required to be small, and the goal is that the drug/biologic will be provided in broader and larger community clinical settings, including rural areas.
Comment: Commenters stated that a CED decision would discriminate against patients with Alzheimer’s disease because CMS has previously covered treatments for conditions such as HIV and cancer that had been approved by the FDA under accelerated approval.
Response: In 2019, CMS considered and issued an NCD on a drug that was approved by the FDA through a similar breakthrough therapy designation (which may also include a surrogate endpoint considered reasonably likely to predict a clinical benefit). For CMS, the emphasis is on the evidence of the association between the surrogate endpoint and clinical outcome. For other accelerated approval drugs for diseases like cancer or HIV, unlike antiamyloid mAbs, there is scientific evidence that the surrogates are directly affect the clinical outcomes or ideally there is evidence that the surrogate is embedded within the causal pathway of the disease progression to the clinical outcome such as mortality. For example, there is scientific evidence on and clinical expert acceptance of the association between progression free survival and overall survival for cancer drugs. There are no scientific studies/evidence that reducing beta-amyloid plaque in the brain will reduce the effects of AD by slowing down or maintaining cognition or function or improve survival.
Down Syndrome
Comment: We had a large number of public comments, approximately 1,800, that requested beneficiaries with Down syndrome and other intellectual and developmental disabilities (IDD) have the same access other patients would have to antiamyloid mAbs.
Response: Further, based on public comments, we are not finalizing the patient exclusion criteria in order to allow appropriate access to patient subpopulations that may need treatment based on ongoing research. We recognize the importance of appropriate patient selection including exclusion criteria as reflected in the numerous patient exclusion criteria used in the published randomized trials. However, we believe this is sufficiently addressed in the CED criteria and protocol review and believe these criteria are no longer needed in the NCD language.
PET for Beta Amyloid
Comment: Some commenters expressed concern over the specification in the proposed decision that one beta amyloid PET scan will be covered, if the patient did not previously receive a beta amyloid PET scan. These commenters were aware that this restriction is due to the CED requirements included in the Beta Amyloid Positron Emission Tomography in Dementia and Neurodegenerative Disease NCD (220.6.20), but ask CMS to reconsider this limitation with the final NCD for antiamyloid mAbs.
Response: At this time, the Beta Amyloid Positron Emission Tomography in Dementia and Neurodegenerative Disease NCD (220.6.20) covers a single PET scan in a lifetime. There are other modalities to determine amyloid on the brain such as cerebral spinal fluid (CSF) analysis, however, CMS is considering whether NCD 220.6.20 needs to be revised.
Part B Premiums
Comment: Many commenters expressed their concern with the price of Aduhelm and frustration with the increase in Medicare premiums, stating that Medicare should negotiate the price for these drugs.
Response: As a policy matter, CMS does not consider cost when making an NCD. The Part B premium and drug pricing is outside the scope of this NCD.
Medicaid
Comment: A couple of commenters expressed concern over the proposed decision stating that the restriction of CED would shift coverage of antiamyloid mAbs for the treatment of AD from Medicare to Medicaid.
Response: Because the manufacturer of Aduhelm has entered into and has in effect a Medicaid drug rebate agreement and because Aduhelm also satisfies the definition of a covered outpatient drug, as set forth at section 1927(k)(2) of the Social Security Act (Act), state Medicaid programs are required to cover the drug when used for a medically accepted indication. However, state Medicaid programs could subject Aduhelm to utilization management techniques, such as prior authorization, and medical necessity criteria. As a covered outpatient drug, states may invoice the manufacturer for rebates on the drug, and manufacturers would be required to pay rebates, as appropriate, when dispensed and paid for under the state plan.
However, when Aduhelm or other drugs included in the NCD are non-covered under the terms of the NCD, they are Part D drugs, and by law, Medicaid cannot pay for Part D drugs for full-benefit dually eligible individuals, regardless of whether they are enrolled in a Part D plan. This means that when these drugs are non-covered under the terms of the NCD, regardless of whether a full-benefit dually eligible individual’s Part D plan actually covers the drug, Medicaid cannot cover it and is not a payor of last resort in this circumstance. Therefore, this policy would not shift coverage of these drugs from Medicare to Medicaid for full-benefit dually-eligible individuals.
Miscellaneous
Comment: One commenter asked if any Prior Authorization or Part B Medical Necessity reviews that were approved prior to this NCD being finalized would still be upheld.
Response: CMS will issue these instructions after the final NCD is published. This final NCD is binding on all MAC coverage determinations from the effective date of this decision, that is the date the NCD is made public.
IX. CMS Analysis
Introduction
National coverage determinations (NCDs) are determinations by the Secretary with respect to whether or not a particular item or service is covered nationally by Medicare (§1869(f)(1)(B) of the Act). In order to be covered by Medicare, an item or service must fall within one or more benefit categories contained within Part A or Part B, and must not be otherwise excluded from coverage. Moreover, with limited exceptions, the expenses incurred for items or services must be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member (§1862(a)(1)(A) of the Act).
In addition to §1862(a)(1)(A) of the Act, a second statutory provision may permit Medicare payment for items and services in some circumstances. That statute, section 1862(a)(1)(E) of the Act, provides, in pertinent part, that:
(a) Notwithstanding any other provision of this title, no payment may be made under part A or part B for any expenses incurred for items or services—
. . .
(1)(E) in the case of research conducted pursuant to section 1142, which is not reasonable and necessary to carry out the purposes of that section.
Section 1142 of the Act describes the authority of the AHRQ to conduct and support research on outcomes, effectiveness, and appropriateness of services and procedures to identify the most effective and appropriate means to prevent, diagnose, treat, and manage diseases, disorders, and other health conditions. That section includes a requirement that the Secretary assure that AHRQ research priorities under Section 1142 appropriately reflect the needs and priorities of the Medicare program.
CED is a paradigm whereby Medicare covers items and services on the condition that they are furnished in the context of approved clinical studies or with the collection of additional clinical data. In making coverage decisions involving CED, CMS decides after a formal review of the medical literature to cover an item or service only in the context of an approved clinical study or when additional clinical data are collected to assess the appropriateness of an item or service for use with a particular beneficiary.
The 2014 CED Guidance Document is available at https://www.cms.gov/medicare-coverage-database/details/medicare-coverage-document-details.aspx?MCDId=27.
When making NCDs, we evaluate the evidence related to our analytic questions based on the quality, strength and totality of evidence presented in the reviewed literature. As part of this evaluation, it is important to consider whether the evidence is relevant to the Medicare beneficiary population. In determining the generalizability of the results of the body of evidence to the Medicare population, we consider, at minimum, the age, race and sex of the study participants.
Evidence Review Summary
For this NCD, CMS focused on the following question:
Is the evidence sufficient to conclude that the use of monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s disease improves health outcomes for Medicare beneficiaries?
The spectrum of Alzheimer’s research
Alzheimer’s disease (AD) is a currently irreversible brain disorder that progressively degrades memory, cognitive function, and ability to carry out tasks of daily living. No Alzheimer’s drug of any type has succeeded, to date, in modifying disease progression. Of all therapies investigated, however, antiamyloid mAbs have been considered by some experts to be amongst the most promising.
The spectrum of AD therapies currently in various stages of investigation extends from antiamyloid, to antitau, neurotransmitter-modifying, cognitive-enhancing, antineuroinflammatory, and neuroprotective therapies (ClinicalTrials.gov 2021, Huang 2020). In 2019 there were a total of 41 trials of AD therapies, with 9 targeting amyloid (including four using antiamyloid mAbs), and 32 using non-antiamyloid therapies (Huang 2020). In this spectrum, therapies that specifically target amyloid are the ones that most directly test the amyloid hypothesis itself (outlined in the Background section). That is, if amyloid is a cause of AD, then treating amyloid early enough in the disease process should substantially delay or possibly halt progression of AD to severe dementia and premature death. The mechanistic strategies of antiamyloid therapies include interrupting Aβ production and/or aggregation, or clearing existing Aβ in the brain. Of these strategies, researchers have increasingly focused on clearing Aβ using antiamyloid mAbs; as one study summarizes, "passive immunotherapy using monoclonal antibodies against Aβ has been best tolerated and, given its mechanistic selectivity, has been widely considered as the therapeutic approach of choice (Panza 2019)" (Avgerinos 2021).
Antiamyloid monoclonal antibodies - quality and strength of evidence
Various dosages of five antiamyloid mAbs were studied in 12 unique trials (see Table 1, Section VII.B, Evidence section), some of which had associated substudies, follow-up studies, or secondary analyses. To date, no large, pivotal RCT, or set of RCTs, of an antiamyloid mAb has been completed, with a trial report published in the peer-reviewed medical literature demonstrating a clear (non-conflicting) improved health outcome (i.e., a meaningful clinical benefit in terms of slowing in the decline of cognition and function) for Medicare beneficiaries with AD. Thus, there is insufficient evidence to conclude that the use of monoclonal antibodies directed against amyloid is reasonable and necessary for the treatment of Alzheimer’s disease under §1862(a)(1)(A) of the Social Security Act. CMS believes that clear evidence about the clinical benefits and harms of any drug in this antiamyloid mAb class is needed for Medicare beneficiaries with early AD to make, along with their physicians and trusted advisors, informed decisions about whether the treatment is appropriate for them.
In what follows, we discuss the quality and strength of the available evidence, focusing on the most recent large, pivotal RCTs for an antiamyloid mAb, the twin EMERGE and ENGAGE trials on aducanumab (Aduhelm™), as this is the only antiamyloid mAb for the treatment of AD that has been approved by the FDA under accelerated approval at the time of this NCD. We then assess the totality of evidence for antiamyloid mAbs through the lens of Coverage with Evidence Development (CED), which provides coverage in the context of research designed to fill important evidence gaps. It is through this CED lens that one can best see the reason for the "class" approach (to treat similar interventions similarly, and provide one standard with a clear but flexible pathway), while also providing that each antiamyloid mAb within the class be evaluated on its own merits, in its own RCTs and CMS-approved studies.
A. Benefits
Any assessment of patient health outcomes must weigh benefits and harms. Historically CMS has focused on improved health outcomes in coverage determinations, including appropriate patient centered outcomes. For these treatments, the goal has been a decline in the slowing of cognition and function due to AD.
The EMERGE and ENGAGE trials
After the Phase 1 PRIME trial of 197 patients (NCT01677572), Biogen launched two identically-designed Phase 3 multicenter, double-blind, RCTs with a total of 3285 patients: ENGAGE (Study 301, NCT02477800) and EMERGE (Study 302, NCT02484547). The trials included patients with a positive PET Aꞵ brain scan, and either MCI due to AD (>80% of trial participants) or mild AD (determined by general patient inclusion criteria of a global Clinical Dementia Rating [CDR] score of 0.5, and a Mini–Mental State Examination score ranging from 24 to 30). (FDA 2021, Rabinovici 2021, ClinicalTrials.gov 2021.) Patients were randomized 1:1:1 to low-dose aducanumab, high-dose aducanumab, or placebo. In the final protocol version, while the low-dose varied by APOE ɛ4 positive or negative, all patients in the high-dose groups received 10 mg/kg.
The primary outcome of interest (or endpoint) in both trials was a change from baseline in the CDR Sum-of-Boxes score (CDR-SB). A CDR-SB is "an 18-point scale measuring cognition (memory, orientation, judgment, and problem solving) and function (community affairs, home and hobbies, personal care)" (Rabinovici2021).
According to the FDA, "Both studies were stopped prior to completion by the independent data monitoring committee (IDMC) after meeting pre-specified futility criteria based upon an analysis of pooled study data (with approximately 57% of patients completing the 78-week treatment period)." The FDA continues, "After the studies were unblinded, it was discovered that Study 302 [EMERGE] had met criteria for statistical significance for the primary endpoint, while Study 301 [ENGAGE] showed no suggestion of an effect of drug on the primary endpoint" (FDA 2021). The FDA describes these analyses as “in essence, post-hoc analyses” (FDA 2021).
Specifically, for Study 302 [EMERGE], the additional data collected after official halting of the trials (due to prespecified futility criteria) found that "the primary endpoint, evaluating the high dose, was statistically significant with a CDR-SB change from baseline relative to placebo of -0.39 (p=0.0120); the low dose had a non-statistically significant numerical reduction (p = 0.0901)" (FDA 2021). The analysis also reported that Study 302 [EMERGE] met statistical significance for other, secondary outcomes assessing cognition and function: ADAS-Cog-13 and ADCS-ADL-MCI.
In contrast, as described in a publication by one of the members of the FDA’s Peripheral and Central Nervous System Drugs Advisory Committee, "Study 301 [ENGAGE] detected no difference from placebo in either the high-dose or the low-dose group, with participants in the high-dose group having nominally worse cognitive function after 18 months than those in the placebo group. Study 302 [EMERGE] was retrospectively deemed partially successful because a statistically significant, but very small absolute, difference was detected on the primary clinical outcome measure between the high-dose group and the placebo group, with no such difference in the low-dose group" (Alexander 2021). The Advisory Committee’s vote on aducanumab on November 6, 2020 was: 10 against approval, 0 for approval, 1 abstention.
B. Harms
Trial data collected by Biogen helped shine a light on harms associated with use of the drug. This evidence was both reported to the FDA and has appeared in the medical literature. Harms associated with use of an antiamyloid mAb include headaches, dizziness, falls, and amyloid-related imaging abnormalities (ARIA). At the time of this writing, there is ongoing assessment of whether the use of an antiamyloid mAb has caused or contributed to death.
Detected on brain MRI scans, ARIA has two principle forms: vasogenic edema (ARIA-E; essentially swelling of the brain) and intracerebral hemorrhage (ARIA-H; bleeding in the brain). Specific drug type and dose, as well as patients’ apolipoprotein (APOE) ɛ4 carrier versus non-carrier status (Salloway 2018), appear to be associated with occurrence of ARIA. In a recent analysis of safety data of two Phase 3 clinical trials (EMERGE and ENGAGE), ARIA was found in "approximately 40% of participants in the phase 3 studies of aducanumab, and approximately one-quarter of these patients experienced symptoms" (Salloway 2021). The FDA and others note that this is compared to a finding of ARIA in 10% of patients who received placebo (FDA 2021, Rabinovici 2021).
While many cases of ARIA in clinical trials have been subclinical (producing no symptoms), severe cases causing for example, malignant hypertension and epileptiform activity, have been documented (VandeVrede 2020, Scherlek 2020). CMS recognizes that adverse events are more closely monitored and treated in the context of a clinical trial compared to general practice. Thus, we have concerns at this time about harms associated with drug use in patients who would be treated outside the context of the safety monitoring of a controlled trial.
C. Weighing benefits and harms
We emphasize the need to consider clinical benefits and harms together to best inform patients and providers. While there is more to learn about the harms (e.g., in which patients they are more or less likely to occur, and how to better select, monitor, and manage patients, and treat those with apparent harms), any discussion of harms is only relevant once clear clinical benefit from use of the drug has been established. Here, it has not. As emphasized by multiple public commenters, that is why FDA would not grant approval based upon evidence of efficacy from a direct measure of clinical benefit for aducanumab, and is requiring a Phase 4 RCT to definitively assess its clinical benefit. Clear evidence about both benefits and harms is needed for Medicare beneficiaries with early AD to make, along with their physicians and trusted advisors, informed decisions about whether the treatment is appropriate for them.
Competing views published by experts
There are many published reports and expert opinions on Biogen’s analysis of trial data and its conclusions regarding aducanumab’s effectiveness, weighing the benefits and harms (Knopman 2020, Howard 2020, Lin 2021, Rubin 2021, Mullard 2021, Liu 2021, Alexander 2021, Rabinovici 2021, Karlawish 2021, Dunn 2021, FDA 2021). We note that these critiques and explanations were all published prior to the March 18, 2022 Biogen publication describing the EMERGE and ENGAGE trials (which we address below). All agree that aducanumab effectively clears amyloid (this is clearly reported by the FDA, and was the basis for its approval of aducanumab under the accelerated-approval pathway; FDA 2021). And all agree that the EMERGE and ENGAGE trials, although identically designed and conducted almost in parallel, resulted in conflicting outcomes (as described above).
Most experts publishing in the medical literature believe that there is insufficient evidence to answer the question of clinical benefit. As the FDA states, because the "Phase 3 studies stopped for futility (and the consequent limitations) and the failure to substantiate the one positive study, there is not sufficient support for substantial evidence of effectiveness with respect to clinical benefits for aducanumab to support standard approval" (FDA 2021). The FDA is requiring a Phase 4 RCT to definitively assess the possible clinical benefits of aducanumab.
The differences of opinion in the literature to date thus center not primarily on whether the two trials, EMERGE and ENGAGE, had conflicting results (they do), but why, and what the implications are. For example, some experts have stated that:
- The conflicting outcomes could be explained by differences in the placebo groups of the two trials. The known heterogeneity of patients in early stages of AD could have resulted in chance differences between the placebo (control) groups of the two trials. As such, in the EMERGE trial, the small but statistically significant difference between the intervention and placebo groups could have been due to chance worsening of the placebo group, rather than a positive effect of the drug in the intervention group.
- Analysis based on selective (nonrandomized) data is prone to bias and is at best hypothesis-generating (exploratory) only. Thus, the result of any secondary analysis is insufficient to declare "success" in the face of conflicting prospective RCTs.
Very recently, the American Academy of Neurology noted "[w]hether aducanumab will result in a clinically meaningful slowing of AD symptoms remains to be determined, as does the safety of aducanumab in clinical populations" (Day 2022).
In contrast, Biogen has presented explanations for why belief in the promising results (for the high-dose group) of the EMERGE trial, rather than the disappointing results of the ENGAGE trial, is warranted.
CMS’ assessment
CMS acknowledges that there are competing conclusions that can be drawn from the EMERGE and ENGAGE trial data. Because these conclusions compete with one another, they cannot simultaneously be correct. Thus, because the extant data is insufficient to conclusively establish which of the competing conclusions is correct, additional data is required.
While this NCD decision memorandum was going through final CMS review, Biogen published a paper on the EMERGE and ENGAGE trials in The Journal of Prevention of Alzheimer’s Disease which was accessible on the journal’s website beginning March 18, 2022. We acknowledge that the publication was too late for public commenters on this NCD to review and comment (and too late for published reviews of the paper to appear in other journals).
Nonetheless, CMS reviewed the paper and concluded that the evidence itself is not different from that reviewed extensively by the FDA already; we cited, and quoted from, the current FDA reports in our proposed decision memorandum and continue to do so in this final decision memorandum. Also, we are not aware of any change in the approval status of aducanumab, specifically from FDA accelerated approval (based on evidence of amyloid reduction) to FDA traditional approval (based on a direct measure of clinical benefit). Finally, we are not aware of any decision by the FDA to no longer require a Phase 4 trial to definitively assess the clinical benefit of aducanumab.
In sum, CMS believes there is no new evidence that overturns our proposed assessment, that the evidence is insufficient to conclude that use of antiamyloid mAbs is reasonable and necessary for the treatment of Alzheimer’s disease under §1862(a)(1)(A) of the Social Security Act.
Coverage with Evidence Development (CED)
While there is insufficient evidence to demonstrate that antiamyloid mAbs are reasonable and necessary for the treatment of AD, we acknowledge the burden AD poses for our beneficiaries (it is one of the most burdensome diseases in our Medicare population) and for society as a whole. As discussed in the Background section of this NCD, over 6 million older Americans are believed to have AD, and this prevalence is expected to rise to 14 million by 2060 barring effective interventions. Effective treatments are needed, and because of the early but promising evidence and the immense burden of this devastating disease on the Medicare population, we are finalizing CED to support studies to answer whether antiamyloid mAbs improve health outcomes for patients. We believe that the CED paradigm provides the most appropriate pathway to provide Medicare coverage while additional evidence is developed.
Why the evidence is promising for CED
CMS believes the evidence is promising and supports the use of CED due to a constellation of findings, which include: newer antiamyloid mAbs, such as aducanumab, effectively clear brain amyloid (FDA 2021); the high-dose aducanumab group in the EMERGE trial did in fact demonstrate improvement compared to placebo (discussed above); as reported in a recent NEJM publication (Mintun 2021), another antiamyloid mAb, donanemab, demonstrated an improvement compared to placebo (albeit in a small Phase 2
trial); and a recent meta-analysis by National Institute of Aging (NIA) scientists concluded that existing research "provides moderate support for the continuous development of anti-Aβ monoclonal antibodies as a treatment for AD" (Avgerinos 2021). These findings are all discussed further below. Additionally, we recognize the immense burden AD poses to our Medicare beneficiaries and the degree of difficulty in finding effective treatments for it.
Some antiamyloid mAbs clear brain amyloid
We are unaware of any expert who, in publications or comments, disagrees with the FDA conclusion that at least some newer drugs within this antiamyloid class, including aducanumab, are effective in reducing brain amyloid; this is the basis for the FDA accelerated approval of aducanumab (FDA 2021). However, there is no convincing evidentiary link between clearance of amyloid and meaningful clinical benefit (an improved health outcome); and here again we agree with the FDA and academic experts (FDA 2021, Ackley 2021). The importance attributed to brain amyloid clearance derives from the amyloid hypothesis, which underpins all antiamyloid trials. Again, if amyloid is a cause of AD, then treating amyloid early enough in the disease process should substantially delay or possibly halt progression of AD to severe dementia and premature death.
This NCD does not, however, draw conclusions one way or the other about the veracity of the amyloid hypothesis. Trial results should ultimately determine its fate.
High-dose aducanumab might improve health outcomes
When data was collected and analyzed for the EMERGE high-dose aducanumab group, it demonstrated a statistically significant improvement compared to the placebo group (discussed above). While uncertainty remains (in part because of the selective nature of this assessment, and the conflicting results of the twin EMERGE and ENGAGE trials), we nonetheless believe that timely completion of a well-designed Phase 4 RCT is appropriate to provide clear answers about benefits and harms for aducanumab.
The Phase 2 trial of donanemab is promising
The Phase 2 RCT on donanemab, published in the New England Journal of Medicine (NEJM), demonstrated a statistically significant relative improvement of the treated group compared to the placebo control group (Mintun 2021). With respect to the primary outcome, the "change from baseline in the iADRS [Integrated Alzheimer's Disease Rating Scale] score at 76 weeks was −6.86 in the donanemab group and −10.06 in the placebo group (difference, 3.20; 95% confidence interval [CI], 0.12 to 6.27; P = 0.04) (Fig. 2A and Table S3); a smaller reduction indicates less cognitive and functional decline" (Mintun 2021). While there are important questions raised in the editorial accompanying the trial report in the NEJM (Levey 2021), and by other experts and commenters, we note that the purpose of such smaller Phase 2 trials is relatively modest. The aim is not to definitely demonstrate clinical benefit, but rather to resolve dosing issues, and determine whether a larger, pivotal Phase 3 trial is worthwhile, and if so, how best to design it. That much larger, pivotal trial of donanemab is well underway, and we look forward to seeing its results, as well as the results of other emerging large, pivotal Phase 3 RCTs for antiamyloid mAbs such as lecanemab and gantenerumab.
Meta-analysis provides "moderate support" for further research
A recent meta-analysis of antiamyloid mAb Phase 3 trials, performed by scientists at the NIA, found evidence of statistical significance, but not necessarily clinically meaningful differences in health outcomes, concluding that the existing research "provides moderate support for the continuous development of anti-Aβ monoclonal antibodies as a treatment for AD." The authors cautioned that any conclusions drawn from the meta-analysis should be considered preliminary, and individual trials are needed to determine the clinical effectiveness of each antiamyloid mAb for the treatment of AD. As they state, "The generated evidence [from this meta-analysis] cannot be used to substitute or supersede the analysis of individual trials."
Revision of proposed CED based on public comments
The above reasons explain why we are providing coverage with CED (as opposed to national non-coverage). Informed by public comments, the structure and focus of this CED for antiamyloid mAbs is similar to, but has evolved from, our January 2022 proposed NCD and decision memorandum. Many commenters agree with the FDA (and the CMS proposed decision) that there needs to be clear (nonconflicting) evidence of clinical benefit associated with use of an antiamyloid mAb for patients with early AD. Commenters point out that this is why the FDA could not grant traditional approval to aducanumab (based upon evidence of efficacy from a direct measure of clinical benefit) and is requiring a Phase 4 RCT to definitively assess its clinical benefit (as discussed earlier).
There is also strong support for CMS to allow FDA "to do its job" of working with manufacturers on trial designs with no requirement that CMS get involved, including to review these protocols. This coincides with the reality that RCTs designed for FDA approval for the well-known antiamyloid mAbs (aducanumab, donanemab, lecanemab, gantenerumab) are far enough along that the companies themselves generally do not need or want CMS support for their trials. They also want reassurance that there will be no duplication of RCTs already performed for the FDA (which was not the intent of the proposed decision).
Commenters also want CMS, if it does require CED (and some of these commenters are for, and some against, CED as their preferred option), to follow a more "traditional" CED structure, and specify the exact questions CED studies must answer in order to achieve full coverage under §1862(a)(1)(A). Most want a transparent process that is as predictable as possible, even while they may disagree with each other and/or CMS on the substance of any given CMS coverage decision.
To address all of these concerns, and others (see detailed responses to public comments), CMS is finalizing this NCD with the following:
- CMS is not requiring a separate RCT that duplicates an RCT conducted for FDA approval. CED will cover a manufacturer’s antiamyloid mAb approved by the FDA for the treatment of AD based on evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) in a RCT conducted under an investigational new drug (IND) application – if that manufacturer wants such support.
- If support is requested, CMS does not need to approve the trial protocol already approved by the FDA, but does need to coordinate the CMS payment operationally, to ensure that payment is administratively feasible for an RCT that is double-blind, placebo-controlled (e.g., so that a "statement of benefits" does not inadvertently unblind patients, and thereby compromise the integrity of the trial).
- Antiamyloid mAbs indicated for the treatment of AD are covered when furnished according to the FDA approved indication in trials supported by the National Institutes of Health (NIH).
- Antiamyloid mAbs that are approved by the FDA for the treatment of AD based on evidence of efficacy from a direct measure of clinical benefit (the current requirement for "traditional approval") are eligible to be covered in CMS-approved prospective comparative studies to answer the CED questions (specified below). These questions are designed to fill key evidence gaps for our Medicare population that remain after these initial RCTs succeed.
What constitutes a "meaningful clinical benefit" in an RCT designed for FDA approval is defined by the current guidance that the FDA applies to all its pivotal trials for AD (FDA 2018; Liu 2021). "Prospective comparative studies" may include a variety of study designs ranging from observational comparative studies to pragmatic randomized trials, and all study data may be collected in a registry. The degree of rigor in the CED study design for a particular antiamyloid mAb will be determined in large part by the strength of evidence in the initial, successful trial(s) designed for FDA approval of that particular drug. Each CMS-approved prospective comparative study must be representative of the diversity of the national population diagnosed with AD. These requirements are all discussed in further detail below.
It is only these prospective comparative studies, designed to answer the CED questions, after the antiamyloid mAb has been FDA approved for the treatment of AD based on the evidence of efficacy from a direct measure of clinical benefit, that require protocol review and approval by CMS – not any of the trials by NIH or in FDA IND applications that CMS supports under this decision.
Summary of the purpose of CED
With the above remarks about evidence and changes to the proposed decision memorandum based on public comments, what follows is a general overview of the threefold purpose of this CED:
- CMS wants to support, without interfering with, FDA and NIH trials of FDA-approved antiamyloid mAbs when that support is wanted.
- When an antiamyloid mAb demonstrates evidence of efficacy from a direct measure of clinical benefit for a selective population in one or more large, pivotal RCTs (Phase 3 or 4), and obtains FDA approval, CMS wants Medicare beneficiaries who are similar to those trial patients to have expeditious access to that biologic.
- Along with this appropriate access, CMS wants simultaneous collection of data for studies that answer key questions (the CED questions below) essential for Medicare beneficiaries and their referring and treating physicians to make informed, appropriate decisions about use of the drug.
This NCD takes a class approach (similar to what CMS did in the CAR-T and PET beta-amyloid NCDs (see sections 110.2 and 220.2.20 of the NCD manual, respectively), in order to establish a predictable pathway to national coverage that applies to every drug in this particular antiamyloid mAb class. At the same time, as each antiamyloid mAb in this class may have a distinct mechanism of action resulting in a distinct benefit/risk profile, each will be evaluated on its own merit in its own studies. This position on individual drug evaluation has been consistently promoted by manufacturers and other experts; we agreed in our proposed decision, and continue to agree in this final decision. Our approach of evaluating each antiamyloid mAb independently is similar to that taken by the FDA in that each antiamyloid mAb is evaluated in its own RCTs for the FDA; similarly, each antiamyloid mAb that has demonstrated a clinical benefit must have studies that answer all of the CED questions (below) in prospective comparative studies for CMS.
Protocols for the prospective comparative studies designed to answer the CED questions must be submitted to CMS for approval, and CMS will work closely with investigators during the study design process.
CED questions
Each CMS approved prospective comparative study must address all of the following questions for Medicare beneficiaries with a clinical diagnosis of mild cognitive impairment (MCI) due to AD or mild AD dementia:
- Does the antiamyloid mAb provide meaningful clinical benefit (i.e., slowing in the decline of cognition and function) in broad community practice?
- Do benefits, and harms such as brain hemorrhage and edema, associated with use of the antiamyloid mAb, depend on characteristics of patients, treating clinicians, and settings?
- How do the benefits and harms change over time?
Medicare beneficiaries and their referring physicians should know if they can expect to achieve similar clinical benefit in their usual care settings, in broad community practice, outside the rigors of clinical trials conducted at relatively few major centers (question #1). As noted in Appendix A, the applicability of the results of a study, in a broader perspective, to other populations, settings, treatment regimens and outcomes assessed is known as external validity. Generalizability to the Medicare population and care settings has been an important consideration in national coverage analyses. Even well-designed and well-conducted trials may not supply the evidence needed if the results of a study are not applicable to the Medicare population. For example, as identified by the study inclusion criteria and often extensive exclusion criteria, the patients enrolled in initial randomized controlled trials designed for demonstrate efficacy are generally healthier than patients usually seen in general community practice. Medicare patients often have multi-comorbidities and are receiving multiple drug treatments. Evidence that provides accurate information about a population or setting not well represented in the Medicare program would be considered but would suffer from limited generalizability. For example, care provided in clinical trial sites and settings often have more immediate access to medical specialists, advanced imaging and emergency care for adverse events compared to the general care settings where usual care is provided in community practice. These factors may have a significant impact on patient selection and management.
It is also important to assess if trial results – benefits and harms alike – depend on certain patient characteristics (question #2) such as demographics, genetics, comorbidities such as hypertension and diabetes, and disease state such as MCI v. mild dementia. That is, the drug may prove to be more or less effective, and entail greater or fewer risks, depending on the characteristics of a given subpopulation. Assessment of subpopulations are often done as part of the trial report, and/or in prespecified substudies and secondary published analyses of trial data. This may entail formal subgroup analysis, sometimes fully powered up front in the trial design (through a larger number of trial participants than would otherwise be the case) in order to provide definitive conclusions (e.g., ‘the treatment works convincingly in MCI patients, but not in those with mild dementia’).
Finally, Medicare beneficiaries should know whether the benefit/harm profile changes over time (question #3).
Other research needs to be conducted to help fully inform patient treatment decisions. Since the evidence on these drugs is still evolving, it is important to address when antiamyloid mAb treatment should be tapered or discontinued and what is the duration of treatment effect. These are often CED questions for treatments that have a more substantial evidence base. We believe that manufacturers and researchers have sufficient incentive to answer these questions in appropriately designed longer term studies. Due to the extended follow-up that may possibly be needed, we are not requiring these questions but would highly encourage the development of such evidence for patient treatment decision making. In addition, there may be subpopulations that are important to study such as individuals with Down syndrome. CMS supports NIH and other federal agency trials in a broad range of clinical topics. Specifically, for patients with Down syndrome, CMS under its clinical trial policy (see Section 310.1 of the NCD manual or https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?ncdid=1&ncdver=2&chapter=all&sortBy=title&bc=18) may cover the routine and related items and services in trials that meet the criteria in the CTP.
Finally, as some have stated during the public comment period, better patient outcomes may be achieved in the future with combinations of AD drugs, along with lifestyle changes and aggressive treatment of known risk factors for AD. We believe this CED is a positive step toward that goal.
CED study protocols
CMS approved CED studies must meet all of the standard CED criteria. There are specific aspects that are important to note for CED protocols under this NCD.
For all CMS-approved studies, the protocol, including the analysis plan, must include:
- A study population:
- whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia; and
- that is consistent with the patient criteria discussed below.
- A neurocognitive evaluation and instruments to assess cognition and function for the clinical diagnosis of MCI due to AD or mild AD dementia for study enrollment and outcomes assessment.
- A description of:
- The multidisciplinary dementia team and optimal medical management.
- Study sites with clinical expertise and infrastructure to provide treatments consistent with the safety monitoring outlined in the FDA-approved label.
Diversity of patients
Given the disappointing lack of inclusion of underserved populations in past trials, we continue to highlight the CED criterion in Section I that requires enrollment of a study population whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia. This has been a longstanding CED requirement, and we are adding this as an explicit key protocol requirement as well. We discuss health disparities in further detail below.
Significant differences in the prevalence of AD across racial and ethnic groups have previously been reported. Research has shown that AD is more prevalent in Blacks and Hispanics when compared to Whites, with Blacks being up to two times more likely to have AD and other dementias when compared to Whites, and Hispanics being about one and a half times more likely than Whites to have AD and other dementias (AA 2020, Mayeda 2016). Despite the higher prevalence of AD and other dementias in Blacks and Hispanics, they are less likely to have a diagnosis when compared to Whites. In a recent survey by the Alzheimer’s Association (2021), it was found that Black, Hispanic, and Native Americans were twice as likely than Whites to say they would not see a doctor if experiencing thinking or memory problems. This can partially be explained by differing racial and ethnic beliefs about AD. Significantly more Black and non-White Americans believe that symptoms of AD, such as significant memory loss, are part of the normal aging process when compared to White Americans (AA 2021, Connell 2009). This may also be partially due to higher rates of discrimination when seeking dementia-related health care. Recent surveys reveal that Blacks reported the highest level of discrimination in dementia health care (50%), followed by Native Americans (42%), Asians (34%), and Hispanics (33%), compared to Non-Hispanic Whites (9%) (AA 2021).
Additionally, under-representation of members of racial and ethnic groups in research relating to AD further exacerbates disparities in our understanding of, and ability to provide appropriate health care for, all individuals CMS serves related to these conditions. Some barriers to the recruitment of under-represented patients can include language, logistical barriers (e.g., time, travel), and a long-standing mistrust of the medical establishment (Watson 2014). In the same survey previously mentioned by the Alzheimer’s Association (2021), 62% of Black Americans believed that medical research is biased against people of color, and Black Americans expressed less interest in participating in clinical trials for AD than any other group surveyed (White and non-White). Additionally, only 53% of Black Americans surveyed believed that a future cure for AD would be equally shared regardless of race and ethnicity.
While these barriers can present a challenge when recruiting under-represented patients for AD research, they may also present challenges related to appropriate diagnosis, management, and care for populations and communities served by CMS. In order to address these barriers in coverage and care, it is critical that these patients are engaged, recruited, and retained in future trials. Due to the lack of diversity in previous trials, the higher prevalence of AD in Black and non-White Americans, and the directives in Executive Order 13985, Advancing Racial Equity and Support for Underserved Communities Through the Federal Government, CMS is finalizing as a study requirement that the diversity of patients included in each study must be representative of the national population diagnosed with AD.
Patient criteria
Based on feedback during the public comment period, we are maintaining the patient inclusion criteria, but removing the patient exclusion criteria, that we had proposed in January, 2022, for CMS-approved studies under CED.
Maintenance of proposed patient inclusion criteria
To enroll, CMS proposed that patients must have:
(i) A clinical diagnosis of mild cognitive impairment (MCI) due to AD or mild AD dementia; and
(ii) Evidence of amyloid pathology consistent with MCI due to AD or mild AD dementia.
We proposed the above criteria because these reflect the general trend in antiamyloid mAb trials of enrolling patients at earlier stages of disease who also meet biomarker criterion. These were the patient inclusion criteria used in the latest antiamyloid mAb Phase 3 trials (EMERGE and ENGAGE). The original, failed trials, such as for bapineuzumab and solanezumab in 2014, targeted primarily patients with dementia. Recent trials have shifted their targets earlier in the disease process, primarily to patients with MCI. This is because antiamyloid experts believe that interventions in later stages of disease (moderate to severe dementia especially) are too late: at that point amyloid has already triggered downstream processes such as pathologic tau accumulation, inflammation, and neurodegeneration. Once triggered, these downstream processes likely cannot be reversed by clearing amyloid.
The proposed decision noted that the shift to earlier stages of disease, while appropriate, directly impacts the consideration of benefits and harms. Because these same patients with early disease are generally high functioning, it is especially important to assess the long-term sequelae of adverse events such as brain hemorrhage and edema (ARIA-H and ARIA-E).
Recent trials requiring biomarker evidence of amyloid pathology for patient enrollment generally have used PET Aꞵ brain scans. The importance of this requirement is exemplified by early, failed solanezumab trials. An analysis of secondary outcomes reported that roughly 25% of trial participants may never have had AD (Siemers 2016). A treatment aimed at improving cognition and function for AD patients, precisely because it modifies underlying AD pathophysiology, is not likely to succeed if it is not AD from brain amyloid that is causing the patients’ symptoms in the first place. In addition to PET Aꞵ brain scans, other evidence-based methods to detect AD pathology will be considered if supported by the peer-reviewed, published medical literature.
Assessment of potential study participants for early AD (MCI due to AD, or mild AD dementia) must involve, in addition to biomarker evidence of AD, a guideline-directed diagnostic work-up that excludes other diseases as a cause of the patient’s symptoms, and use of validated tests to measure cognition and function. Examples of such validated tests include the Montreal Cognitive Assessment (MoCA), the Mini-Mental State Exam (MMSE), and the Clinical Dementia Rating (CDR) scale, all of which are well-supported in the literature and widely used in AD trials. Similarly, primary outcome measures of cognition and function included in protocols for CMS-approved CED studies must be well-supported by the medical literature.
The patient inclusion criteria specified above reflect the minimum inclusion criteria required for CMS approved studies. Based on our review of recent trials (e.g., a recent antiamyloid mAb trial report, Mintun 2021, had 7 inclusion criteria), we anticipate that patient inclusion criteria in protocols submitted to CMS for CED consideration may be more extensive than the criteria proposed above.
Elimination of proposed patient exclusion criteria
In the proposed decision in January, 2022, we listed the following exclusion criteria:
- Any neurological or other medical condition (other than AD) that may significantly contribute to cognitive decline.
- Expected death from any cause during the duration of the study.
- Medical conditions, other than AD, likely to increase significant adverse events.
The first two requirements above (i-ii) were included because they reflect major exclusions commonly seen in AD trials generally. They are also similar to two of the exclusion criteria (of the original protocol’s exclusion list) from the Mintun 2021 NEJM trial publication, the design for which incorporated lessons learned from past failed trials.
The third requirement (iii) was to ensure patient protection. Enrolling patients with medical conditions that may lead to significant adverse events also may complicate or undermine the investigators’ ability to perform the trial and analyze a sufficient amount of completed trial data, which could compromise reliability of the results of the trial as a whole.
However, in this final decision we are eliminating exclusion criteria for CED studies, based on reassessment after extensive feedback during the public comment period. While we will scrutinize patient exclusion criteria proposed in protocols by CED investigators, both for study participant safety and study design integrity, specific exclusions may vary widely depending on what question is being answered for which intended population.
Our goal in this final decision is to leave maximum flexibility for study investigators to conduct a potentially wide range of study designs to assess benefits and harms in special populations (e.g., Down syndrome), and/or patients with various comorbidities who were excluded from the highly-selective patient populations in RCTs designed for FDA approval. Such CED studies may choose to include, for instance, patients with comorbidities that might significantly contribute to mixed dementia. As noted in our Background section, the impact of these mixed diseases on cognition and functioning may be separate and additive, although "it is uncertain whether multiple mixed pathologies act independently or synergistically on risk of all cause dementia" (Brookmeyer 2018).
The implication, again, is that any treatment targeting amyloid specifically may be less effective the greater the level of mixed disease in a given patient. As such patients are generally excluded in the highly-selective RCTs designed for FDA approval, meaningful clinical benefit must be demonstrated for such patients in appropriately designed CED studies in order for these patients to be reflected in positive national coverage criteria. For these reasons, CMS is finalizing the propose inclusion criteria, but removing the proposed requirement of specific exclusion criteria.
Neurocognitive evaluation
Validated cognitive and functional assessment instruments in CED studies
Measurement instruments to be used in the CED studies must have been independently validated and used in prior trials. The rationale for the choice of validated cognitive and functional instruments must be documented in the study protocol. As part of our evidence review, a CMS contractor (ICA) conducted an environmental scan and identified validated cognitive and functional instruments. They reported: "Among the identified 16 trials included in the environmental scan (ES), 78 total instruments (26 unique) were used. The most often cited were the Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog, includes 11-13 item version; n=16, 20.6%), the Mini-Mental State Examination (MMSE; 12, 15.4%), and the Clinical Dementia Rating-Sum of Boxes (CDR-SB; n=9, 11.5%)." As shown in our evidence table 1, the EMERGE and ENGAGE trials used CDR-SB while other drug trials have used ADAS-Cog.
The CED studies must include a neurocognitive evaluation and instruments to assess cognition and function for the clinical diagnosis of MCI due to AD or mild AD dementia for study enrollment and outcomes assessment. It is important that patients are carefully diagnosed before enrollment to ensure that appropriate patients are enrolled for treatment and to establish a baseline for outcomes assessment after antiamyloid mAb treatment.
Medical specialists and clinical expertise
Optimal medical management for mild AD and known risk factors
As noted in the background, the Lancet Commission (reported by Livingston et al., 2020) noted several important modifiable risk factors for dementia prevention, intervention and care. Given the prevalence of multiple comorbidities in Medicare beneficiaries, the recommendations are especially pertinent. For example, mixed dementia, AD and vascular dementia is a common type of dementia in older adults. Optimal medical management would include the conditions associated with vascular dementia including hypertension, diabetes, dyslipidemia and obesity. There may also be medical conditions that may impact results of neurocognitive testing and should also be appropriately managed.
Patients in CMS approved trials and studies under this NCD must be on optimal medical management especially for known risk factors for cognitive and functional decline that lead to dementia, consistent with the Lancet Commission report to include but not limited to hypertension, diabetes, depression, excessive alcohol misuse and smoking.
Multidisciplinary team
The American Academy of Neurology (AAN) recently published a review of the current evidence and clinical practice guidelines (Day et al., 2022). In addition to the review of the evidence, the AAN noted important considerations for involvement of a multidisciplinary dementia team and needed clinical infrastructure. These recommendations were also noted by commenters to the proposed NCD and reported in numerous publications. As one example, Grand and colleagues (2011) reported:
"The best approach to the care of individuals affected by dementia includes support from multiple sources. These may be integrated, parallel, or a combination of both. It is ideal for patients and caregivers to seek a blend of multidisciplinary services that come from various healthcare providers, social service agencies, and professionals from outside the field of healthcare. Multidisciplinary teams vary in their composition and may be structured either formally or informally. Team construction is usually dictated by resources, including time, availability, finances, and geographic location. Regardless of structure, successful teams are characterized by a shared commitment to quality care and an appreciation for the contributions of each team member.
Multidisciplinary teams involved in dementia care tend to be based primarily on the availability of service resources, in addition to the social and cultural context of the community. Team members often include neurologists, geriatricians, neuropsychologists, nurse practitioners, physical/occupational therapists, nutritionists, and social workers."
Clinical infrastructure (settings)
As noted above, one of the most important aspects of generalizability, in addition to patient comorbidities and potential interaction with concomitant treatments, is the care environment where treatments and follow-up care are provided. Often the clinical research sites where treatments are provided in the context of a RCT are substantially different from the general practice settings where much of usual medical care is provided (community practice outside the RCT setting). In addition to the medical staff, there are considerations for the care centers themselves.
To help ensure harms remain acceptable and consistent with current trial evidence, the AAN (Day 2022) also noted important considerations in providing mAb treatment: "The safe prescription of aducanumab will require substantial investment in human and physical infrastructure. The approval of therapies for patients with early symptomatic AD are expected to markedly increase demand for clinicians with appropriate training in the assessment and staging of patients with AD and interpretation of AD biomarker results. Clinics may need to increase capacity for lumbar punctures to assess CSF-based measures of amyloid-β, particularly in rural communities where PET imaging is less available. Clinical capacity will also need to grow to accommodate follow-up visits to assess treatment response and evaluate potential AEs. This increase in demand will further strain the neurology workforce, potentially compromising access to care, patient outcomes, and career satisfaction. Demands will likewise increase for outpatient infusion center space, specialized nursing services to ensure safe administration of aducanumab and patient monitoring, and radiologists and neurologists trained to diagnose ARIA."
Prospective comparative studies and a national registry
We recognize that waiting for published results of an RCT may limit access. However, it is appropriate access that matters and we have real concern about potential harms to Medicare patients, especially since patients in these trials have early or mild disease (MCI or mild AD) and are relatively high functioning. It is important to first demonstrate that the benefits outweigh the harms within the patient protections and controlled settings of RCTs. In finalizing this NCD, CMS has changed the categorical term used to describe CED studies, designed to answer the CED questions, from "prospective longitudinal studies" (in the proposed decision) to "prospective comparative studies" (in this final decision) due to the comparison group. All CMS-approved studies must adhere to the standards of scientific integrity (CED criteria a-m) that have been identified by the Agency for Healthcare Research and Quality (AHRQ).
This approach strikes an appropriate balance of providing patient access while also ensuring both protections for patients from harms and the appropriate data collection and analysis to address CMS’ questions to determine whether CMS should undertake an NCD reconsideration.
We note that a registry is not itself a study; it is a vehicle for collection of harmonized data with standardized definitions of terms. There can be broad access to this data, and that data can be analyzed in virtually any type of study or trial prospectively embedded into the registry design.
CED study designs depend on strength of trial evidence (see Appendix A)
As mentioned above, the degree of rigor in study designs to answer CED questions may depend in good part on the strength of evidence (Appendix A) of the initial RCT that led to FDA approval. Generally, the stronger the evidence in the initial trial (including any prespecified extensions of the trial, substudies, follow-up studies, or secondary analyses of trial data), the less the rigor needed in studies to answer the CED questions.
Figure 1. Strength of Evidence (Illustrative Purposes Only)
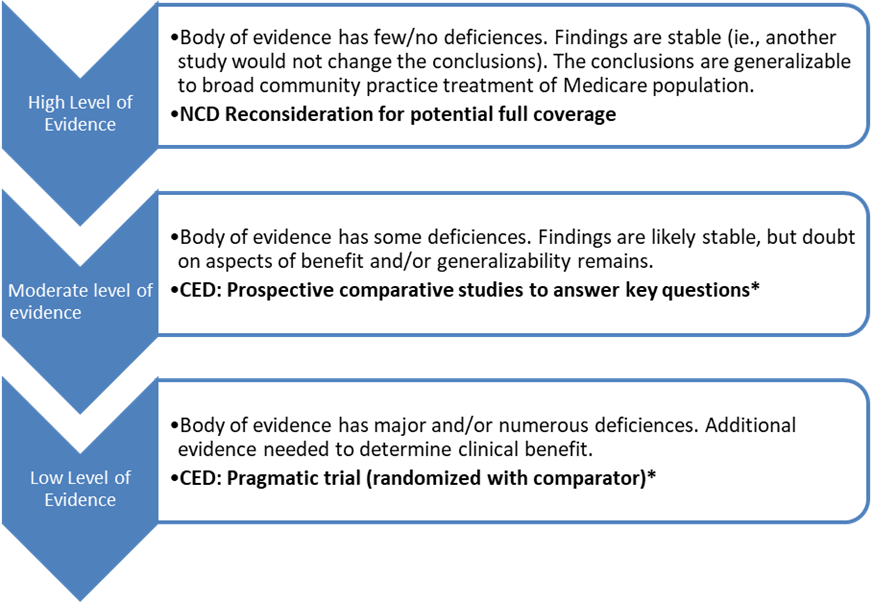
What constitutes "strength of evidence" (Appendix A)
As for what constitutes "strength of evidence," the analyses in all our NCDs have explicitly assessed the quality and overall strength of evidence for the medical item or service in the accessible, peer-reviewed, medical literature (see appendix A for detailed discussion). With access to the publications, the public sees what we see. In turn, the peer-review process is part of evidence-based medicine itself.
CED can support expanded indications/subpopulations
In the scenario where treatment is sought for patients who are substantially different from those participants included in the initial RCTs designed for FDA approval, then evaluation would require greater rigor, such as with a pragmatic RCT. Use of pragmatic clinical trials was strongly recommended by some public commenters during the public comment period. Pragmatic trials could be quite large, and involve broad community care settings (e.g., outside of major centers and hospitals). Such trials could rigorously answer whether the clinical benefit seen in the initial RCTs are replicable in broad community practice, when certain major inclusion and exclusion criteria of the FDA-approved RCT are relaxed.
Thus, appropriate CED study design could assess whether benefits, and also harms such as brain swelling and bleeding (associated with ARIA), are the same, reduced or increased when the treatment is used in broader community practice, in a different patient population (with major trial inclusion and exclusion criteria relaxed), or both.
The question specifically about generalizability of treatment results to Medicare beneficiaries who are substantially dissimilar to trial participants, is not a formal requirement of this CED. Thus, an antiamyloid mAb may move from CED status to full, national coverage under §1862(a)(1)(A) by answering only the CED questions (1 through 3). However, in this case the national coverage criteria would reflect the major inclusion and exclusion criteria of those initial trials on which the NCD is based.
In sum, CMS is issuing a final NCD that concludes with CED for this particular class of antiamyloid mAbs for the treatment of AD. The reason for CED is that even if the FDA were to determine that an antiamyloid mAb is approved because it demonstrates efficacy from a direct measure of clinical benefit, that approval is based on RCT results according to rigorous clinical trial protocols, in relatively few, advanced care settings such as academic medical centers, conducted with dementia experts, and in a highly-selected patient population that is different (e.g., with fewer co-morbidities) from the general Medicare population. It is important that there is evidence that demonstrates that the positive RCT results for FDA approval are generalizable both to broader community care settings, and to the broader Medicare population that includes patients with co-morbidities such as hypertension, heart disease, diabetes, and the like.
Therefore, at this time, CMS concludes that an FDA determination that an antiamyloid mAb for the treatment of AD demonstrates efficacy from a direct measure of clinical benefit is promising but does not meet the §1862(a)(1)(A) reasonable and necessary statute. Prospective comparative studies designed to answer all of the CED questions, which could range from a large, registry-based study with a comparator to a pragmatic clinical trial, are appropriate coverage for the present time. CMS needs evidence that an antiamyloid mAb for the treatment of AD demonstrates improved health outcomes, with reasonable risk of harm, in broader community practice and in the broader Medicare population, that are similar to results achieved in successful but narrowly-designed RCTs seeking to establish safety and efficacy for FDA approval.
X. Conclusion
Decision
A. The Centers for Medicare & Medicaid Services (CMS) covers Food and Drug Administration (FDA) approved monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s disease
(AD) when furnished in accordance with Section B (Coverage Criteria) under coverage with evidence development (CED) for patients who have:
- A clinical diagnosis of mild cognitive impairment (MCI) due to AD or mild AD dementia, both with confirmed presence of amyloid beta pathology consistent with AD.
B. Coverage Criteria:
1) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) considered as reasonably likely to predict clinical benefit may be covered in a randomized controlled trial conducted under an investigational new drug (IND) application.
2) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit may be covered in CMS approved prospective comparative studies. Study data for CMS approved prospective comparative studies may be collected in a registry.
3) For CMS-approved studies, the protocol, including the analysis plan, must include:
- A study population whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia.
- A neurocognitive evaluation and a description of the instruments used to assess cognition and function for the clinical diagnosis of MCI due to AD or mild AD dementia for study enrollment and outcomes assessment.
- A description of:
- The multidisciplinary dementia team and optimal medical management.
- Study sites with clinical expertise and infrastructure to provide treatments consistent with the safety monitoring outlined in the FDA-approved label.
4) CMS-approved studies of a monoclonal antibody directed against amyloid (antiamyloid mAb) approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit must address all of the questions below:
- Does the antiamyloid mAb meaningfully improve health outcomes (i.e., slow the decline of cognition and function) for patients in broad community practice?
- Do benefits, and harms such as brain hemorrhage and edema, associated with use of the antiamyloid mAb, depend on characteristics of patients, treating clinicians, and settings?
- How do the benefits and harms change over time?
5) CMS-approved studies must adhere to the following standards of scientific integrity that have been identified by the Agency for Healthcare Research and Quality:
- The principal purpose of the study is to test whether the item or service meaningfully improves health outcomes of affected beneficiaries who are represented by the enrolled subjects.
- The rationale for the study is well supported by available scientific and medical evidence.
- The study results are not anticipated to unjustifiably duplicate existing knowledge.
- The study design is methodologically appropriate and the anticipated number of enrolled subjects is sufficient to answer the research question(s) being asked in the National Coverage Determination.
- The study is sponsored by an organization or individual capable of completing it successfully.
- The research study is in compliance with all applicable Federal regulations concerning the protection of human subjects found in the Code of Federal Regulations (CFR) at 45 CFR Part 46. If a study is regulated by the Food and Drug Administration (FDA), it is also in compliance with 21 CFR Parts 50 and 56. In addition, to further enhance the protection of human subjects in studies conducted under CED, the study must provide and obtain meaningful informed consent from patients regarding the risks associated with the study items and/or services, and the use and eventual disposition of the collected data.
- All aspects of the study are conducted according to appropriate standards of scientific integrity.
- The study has a written protocol that clearly demonstrates adherence to the standards listed here as Medicare requirements.
- The study is not designed to exclusively test toxicity or disease pathophysiology in healthy individuals. Such studies may meet this requirement only if the disease or condition being studied is life threatening as defined in 21 CFR §312.81(a) and the patient has no other viable treatment options.
- The clinical research studies and registries are registered on the www.ClinicalTrials.gov website by the principal sponsor/investigator prior to the enrollment of the first study subject. Registries are also registered in the Agency for Healthcare Research and Quality (AHRQ) Registry of Patient Registries (RoPR).
- The research study protocol specifies the method and timing of public release of all prespecified outcomes to be measured including release of outcomes if outcomes are negative or study is terminated early. The results must be made public within 12 months of the study’s primary completion date, which is the date the final subject had final data collection for the primary endpoint, even if the trial does not achieve its primary aim. The results must include number started/completed, summary results for primary and secondary outcome measures, statistical analyses, and adverse events. Final results must be reported in a publicly accessible manner; either in a peer-reviewed scientific journal (in print or on-line), in an on-line publicly accessible registry dedicated to the dissemination of clinical trial information such as ClinicalTrials.gov, or in journals willing to publish in abbreviated format (e.g., for studies with negative or incomplete results).
- The study protocol must explicitly discuss beneficiary subpopulations affected by the item or service under investigation, particularly traditionally underrepresented groups in clinical studies, how the inclusion and exclusion criteria effect enrollment of these populations, and a plan for the retention and reporting of said populations in the trial. If the inclusion and exclusion criteria are expected to have a negative effect on the recruitment or retention of underrepresented populations, the protocol must discuss why these criteria are necessary.
- The study protocol explicitly discusses how the results are or are not expected to be generalizable to affected beneficiary subpopulations. Separate discussions in the protocol may be necessary for populations eligible for Medicare due to age, disability or Medicaid eligibility.
The principal investigator must submit the complete trial protocol, cite where the detailed analysis plan for the CMS CED questions occurs in the protocol, and provide a statement addressing how the study satisfies each of the standards of scientific integrity (a. through m. listed above), as well as the investigator’s contact information, to the email address below. The information will be reviewed, and approved trials will be identified on the CMS website.
Email address for protocol submissions: clinicalstudynotification@cms.hhs.gov Email subject line: "CED Monoclonal Antibodies for the Treatment of Alzheimer’s Disease [name of
sponsor/primary investigator]"
C. Monoclonal antibodies directed against amyloid indicated for the treatment of AD are covered when furnished according to the FDA approved indication in National Institutes of Health (NIH)-supported trials.
D. For any CMS approved study, or NIH-supported trial, that includes a beta amyloid positron emission tomography (PET) scan as part of the protocol, it has been determined that these trials or studies also meet the CED requirements included in the Beta Amyloid Positron Emission Tomography in Dementia and Neurodegenerative Disease NCD (220.6.20).
E. Monoclonal antibodies directed against amyloid for the treatment of AD provided outside of a FDA approved randomized controlled trial, CMS approved studies, or studies supported by the NIH, are nationally non-covered.
Consistent with section 1142 of the Act, AHRQ supports Medicare coverage of FDA trials in Section B.1, NIH trials, and CMS-approved studies that meet all the standards identified above, and address the above-listed research questions.
See Appendix B for the suggested manual language for the National Coverage Determination.
APPENDIX A
General Methodological Principles of Study Design
(Section VI of the Decision Memorandum)
When making national coverage determinations, CMS evaluates relevant clinical evidence to determine whether or not the evidence is of sufficient quality to support a finding that an item or service is reasonable and necessary. The overall objective for the critical appraisal of the evidence is to determine to what degree we are confident that: 1) the specific assessment questions can be answered conclusively; and 2) the intervention will improve health outcomes for patients.
We divide the assessment of clinical evidence into three stages: 1) the quality of the individual studies; 2) the generalizability of findings from individual studies to the Medicare population; and 3) overarching conclusions that can be drawn from the body of the evidence on the direction and magnitude of the intervention’s potential risks and benefits.
The methodological principles described below represent a broad discussion of the issues we consider when reviewing clinical evidence. However, it should be noted that each coverage determination has its unique methodological aspects.
Assessing Individual Studies
Methodologists have developed criteria to determine weaknesses and strengths of clinical research. Strength of evidence generally refers to: 1) the scientific validity underlying study findings regarding causal relationships between health care interventions and health outcomes; and 2) the reduction of bias. In general, some of the methodological attributes associated with stronger evidence include those listed below:
- Use of randomization (allocation of patients to either intervention or control group) in order to minimize bias.
- Use of contemporaneous control groups (rather than historical controls) in order to ensure comparability between the intervention and control groups.
- Prospective (rather than retrospective) studies to ensure a more thorough and systematical assessment of factors related to outcomes.
- Larger sample sizes in studies to demonstrate both statistically significant as well as clinically significant outcomes that can be extrapolated to the Medicare population. Sample size should be large enough to make chance an unlikely explanation for what was found.
- Masking (blinding) to ensure patients and investigators do not know to that group patients were assigned (intervention or control). This is important especially in subjective outcomes, such as pain or quality of life, where enthusiasm and psychological factors may lead to an improved perceived outcome by either the patient or assessor.
Regardless of whether the design of a study is a randomized controlled trial, a non-randomized controlled trial, a cohort study or a case-control study, the primary criterion for methodological strength or quality is to the extent that differences between intervention and control groups can be attributed to the intervention studied. This is known as internal validity. Various types of bias can undermine internal validity. These include:
- Different characteristics between patients participating and those theoretically eligible for study but not participating (selection bias).
- Co-interventions or provision of care apart from the intervention under evaluation (performance bias).
- Differential assessment of outcome (detection bias).
- Occurrence and reporting of patients who do not complete the study (attrition bias).
In principle, rankings of research design have been based on the ability of each study design category to minimize these biases. A randomized controlled trial minimizes systematic bias (in theory) by selecting a sample of participants from a particular population and allocating them randomly to the intervention and control groups. Thus, in general, randomized controlled studies have been typically assigned the greatest strength, followed by non-randomized clinical trials and controlled observational studies. The design, conduct and analysis of trials are important factors as well. For example, a well-designed and conducted observational study with a large sample size may provide stronger evidence than a poorly designed and conducted randomized controlled trial with a small sample size. The following is a representative list of study designs (some of that have alternative names) ranked from most to least methodologically rigorous in their potential ability to minimize systematic bias:
Randomized controlled trials
Non-randomized controlled trials
Prospective cohort studies
Retrospective case control studies
Cross-sectional studies
Surveillance studies (e.g., using registries or surveys)
Consecutive case series
Single case reports
When there are merely associations but not causal relationships between a study’s variables and outcomes, it is important not to draw causal inferences. Confounding refers to independent variables that systematically vary with the causal variable. This distorts measurement of the outcome of interest because its effect size is mixed with the effects of other extraneous factors. For observational, and in some cases randomized controlled trials, the method in that confounding factors are handled (either through stratification or appropriate statistical modeling) are of particular concern. For example, in order to interpret and generalize conclusions to our population of Medicare patients, it may be necessary for studies to match or stratify their intervention and control groups by patient age or co-morbidities.
Methodological strength is, therefore, a multidimensional concept that relates to the design, implementation and analysis of a clinical study. In addition, thorough documentation of the conduct of the research, particularly study selection criteria, rate of attrition and process for data collection, is essential for CMS to adequately assess and consider the evidence.
Generalizability of Clinical Evidence to the Medicare Population
The applicability of the results of a study to other populations, settings, treatment regimens and outcomes assessed is known as external validity. Even well-designed and well-conducted trials may not supply the evidence needed if the results of a study are not applicable to the Medicare population. Evidence that provides accurate information about a population or setting not well represented in the Medicare program would be considered but would suffer from limited generalizability.
The extent to that the results of a trial are applicable to other circumstances is often a matter of judgment that depends on specific study characteristics, primarily the patient population studied (age, sex, severity of disease and presence of co-morbidities) and the care setting (primary to tertiary level of care, as well as the experience and specialization of the care provider). Additional relevant variables are treatment regimens (dosage, timing and route of administration), co-interventions or concomitant therapies, and type of outcome and length of follow-up.
The level of care and the experience of the providers in the study are other crucial elements in assessing a study’s external validity. Trial participants in an academic medical center may receive more or different attention than is typically available in non-tertiary settings. For example, an investigator’s lengthy and detailed explanations of the potential benefits of the intervention and/or the use of new equipment provided to the academic center by the study sponsor may raise doubts about the applicability of study findings to community practice.
Given the evidence available in the research literature, some degree of generalization about an intervention’s potential benefits and harms is invariably required in making coverage determinations for the Medicare population. Conditions that assist us in making reasonable generalizations are biologic plausibility, similarities between the populations studied and Medicare patients (age, sex, ethnicity and clinical presentation) and similarities of the intervention studied to those that would be routinely available in community practice.
A study’s selected outcomes are an important consideration in generalizing available clinical evidence to Medicare coverage determinations. One of the goals of our determination process is to assess health outcomes. These outcomes include resultant risks and benefits such as increased or decreased morbidity and mortality. In order to make this determination, it is often necessary to evaluate whether the strength of the evidence is adequate to draw conclusions about the direction and magnitude of each individual outcome relevant to the intervention under study. In addition, it is important that an intervention’s benefits are clinically significant and durable, rather than marginal or short-lived. Generally, an intervention is not reasonable and necessary if its risks outweigh its benefits.
If key health outcomes have not been studied or the direction of clinical effect is inconclusive, we may also evaluate the strength and adequacy of indirect evidence linking intermediate or surrogate outcomes to our outcomes of interest.
Assessing the Relative Magnitude of Risks and Benefits
Generally, an intervention is not reasonable and necessary if its risks outweigh its benefits. Health outcomes are one of several considerations in determining whether an item or service is reasonable and necessary. CMS places greater emphasis on health outcomes actually experienced by patients, such as quality of life, functional status, duration of disability, morbidity and mortality, and less emphasis on outcomes that patients do not directly experience, such as intermediate outcomes, surrogate outcomes, and laboratory or radiographic responses. The direction, magnitude, and consistency of the risks and benefits across studies are also important considerations. Based on the analysis of the strength of the evidence, CMS assesses the relative magnitude of an intervention or technology’s benefits and risk of harm to Medicare beneficiaries.
APPENDIX B
Medicare National Coverage Determinations Manual
Draft
This information is representative of Medicare's national coverage determination (NCD) for implementation purposes only. The information is subject to formal revisions and formatting changes prior to the release of the final NCD contractor instructions and publication in the Medicare National Coverage Determinations Manual.
Table of Contents
(Rev.)
[XXX.X]
Nationally Covered Indication
The Centers for Medicare & Medicaid Services (CMS) covers Food and Drug Administration (FDA) approved monoclonal antibodies directed against amyloid for the treatment of Alzheimer’s disease (AD) when furnished in accordance with Section B (Coverage Criteria) under coverage with evidence development (CED) for patients who have:
A clinical diagnosis of mild cognitive impairment (MCI) due to AD or mild AD dementia, both with confirmed presence of amyloid beta pathology consistent with AD.
Coverage Criteria:
1) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a change in a surrogate endpoint (e.g., amyloid reduction) considered as reasonably likely to predict clinical benefit may be covered in a randomized controlled trial conducted under an investigational new drug (IND) application.
2) Monoclonal antibodies directed against amyloid that are approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit may be covered in CMS approved prospective comparative studies. Study data for CMS approved prospective comparative studies may be collected in a registry.
3) For CMS-approved studies, the protocol, including the analysis plan, must include:
- A study population whose diversity of patients are representative of the national population with MCI due to AD or mild AD dementia.
- A neurocognitive evaluation and a description of the instruments used to assess cognition and function for the clinical diagnosis of MCI due to AD or mild AD dementia for study enrollment and outcomes assessment.
- A description of:
- The multidisciplinary dementia team and optimal medical management.
- Study sites with clinical expertise and infrastructure to provide treatments consistent with the safety monitoring outlined in the FDA-approved label.
4) CMS-approved studies of a monoclonal antibody directed against amyloid (antiamyloid mAb) approved by FDA for the treatment of AD based upon evidence of efficacy from a direct measure of clinical benefit must address all of the questions below:
- Does the antiamyloid mAb meaningfully improve health outcomes (i.e., slow the decline of cognition and function) for patients in broad community practice?
- Do benefits, and harms such as brain hemorrhage and edema, associated with use of the antiamyloid mAb, depend on characteristics of patients, treating clinicians, and settings?
- How do the benefits and harms change over time?
5) CMS-approved studies must adhere to the following standards of scientific integrity that have been identified by the Agency for Healthcare Research and Quality:
- The principal purpose of the study is to test whether the item or service meaningfully improves health outcomes of affected beneficiaries who are represented by the enrolled subjects.
- The rationale for the study is well supported by available scientific and medical evidence.
- The study results are not anticipated to unjustifiably duplicate existing knowledge.
- The study design is methodologically appropriate and the anticipated number of enrolled subjects is sufficient to answer the research question(s) being asked in the National Coverage Determination.
- The study is sponsored by an organization or individual capable of completing it successfully.
- The research study is in compliance with all applicable Federal regulations concerning the protection of human subjects found in the Code of Federal Regulations (CFR) at 45 CFR Part 46. If a study is regulated by the Food and Drug Administration (FDA), it is also in compliance with 21 CFR Parts 50 and 56. In addition, to further enhance the protection of human subjects in studies conducted under CED, the study must provide and obtain meaningful informed consent from patients regarding the risks associated with the study items and/or services, and the use and eventual disposition of the collected data.
- All aspects of the study are conducted according to appropriate standards of scientific integrity.
- The study has a written protocol that clearly demonstrates adherence to the standards listed here as Medicare requirements.
- The study is not designed to exclusively test toxicity or disease pathophysiology in healthy individuals. Such studies may meet this requirement only if the disease or condition being studied is life threatening as defined in 21 CFR §312.81(a) and the patient has no other viable treatment options.
- The clinical research studies and registries are registered on the www.ClinicalTrials.gov website by the principal sponsor/investigator prior to the enrollment of the first study subject. Registries are also registered in the Agency for Healthcare Research and Quality (AHRQ) Registry of Patient Registries (RoPR).
- The research study protocol specifies the method and timing of public release of all prespecified outcomes to be measured including release of outcomes if outcomes are negative or study is terminated early. The results must be made public within 12 months of the study’s primary completion date, which is the date the final subject had final data collection for the primary endpoint, even if the trial does not achieve its primary aim. The results must include number started/completed, summary results for primary and secondary outcome measures, statistical analyses, and adverse events. Final results must be reported in a publicly accessible manner; either in a peer-reviewed scientific journal (in print or on-line), in an on-line publicly accessible registry dedicated to the dissemination of clinical trial information such as ClinicalTrials.gov, or in journals willing to publish in abbreviated format (e.g., for studies with negative or incomplete results).
- The study protocol must explicitly discuss beneficiary subpopulations affected by the item or service under investigation, particularly traditionally underrepresented groups in clinical studies, how the inclusion and exclusion criteria effect enrollment of these populations, and a plan for the retention and reporting of said populations in the trial. If the inclusion and exclusion criteria are expected to have a negative effect on the recruitment or retention of underrepresented populations, the protocol must discuss why these criteria are necessary.
- The study protocol explicitly discusses how the results are or are not expected to be generalizable to affected beneficiary subpopulations. Separate discussions in the protocol may be necessary for populations eligible for Medicare due to age, disability or Medicaid eligibility.
The principal investigator must submit the complete trial protocol, cite where the detailed analysis plan for the CMS CED questions occurs in the protocol, and provide a statement addressing how the study satisfies each of the standards of scientific integrity (a. through m. listed above), as well as the investigator’s contact information, to the email address below. The information will be reviewed, and approved trials will be identified on the CMS website.
Email address for protocol submissions: clinicalstudynotification@cms.hhs.gov Email subject line: "CED Monoclonal Antibodies for the Treatment of Alzheimer’s Disease [name of sponsor/primary investigator]"
Monoclonal antibodies directed against amyloid indicated for the treatment of AD are covered when furnished according to the FDA approved indication in National Institutes of Health (NIH)-supported trials.
For any CMS approved study, or NIH-supported trial, that includes a beta amyloid positron emission tomography (PET) scan as part of the protocol, it has been determined that these trials or studies also meet the CED requirements included in the Beta Amyloid Positron Emission Tomography in Dementia and Neurodegenerative Disease NCD (220.6.20).
Nationally Non-Covered
Monoclonal antibodies directed against amyloid for the treatment of AD provided outside of the FDA approved randomized controlled trial, CMS approved studies, or studies supported by the NIH, are nationally non-covered.


